Volume 15, Issue 6 (November & December 2024)
BCN 2024, 15(6): 807-818 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Esmaeili S, Taremian F, Rezaei M, Vousooghi N, Mostafavi H. Comparing the Efficacy of Matrix Therapy, Transcranial Magnetic Stimulation, and Cognitive Rehabilitation in Attention Bias Modification and Craving Reduction in Stimulant Drug Users. BCN 2024; 15 (6) :807-818
URL: http://bcn.iums.ac.ir/article-1-2090-en.html
URL: http://bcn.iums.ac.ir/article-1-2090-en.html
1- Department of Clinical Psychology and Addiction Studies, School of Medicine, Zanjan University of Medical Sciences, Zanjan, Iran.
2- Department of Neuroscience and Addiction Studies, School of Advanced Technologies in Medicine, Tehran University of Medical Sciences, Tehran, Iran.
3- Department of Physiology, School of Medicine, Zanjan University of Medical Sciences, Zanjan, Iran.
2- Department of Neuroscience and Addiction Studies, School of Advanced Technologies in Medicine, Tehran University of Medical Sciences, Tehran, Iran.
3- Department of Physiology, School of Medicine, Zanjan University of Medical Sciences, Zanjan, Iran.
Full-Text [PDF 612 kb]
| Abstract (HTML)
Full-Text:
1. Introduction
Addiction is a recurrent and chronic brain disease. According to official UN statistics and the book of world report on drugs, addiction and its consequences and complications accounted for 183000 deaths in 2012. It is estimated that 162 to 324 million people worldwide have used at least one type of addictive drug, such as hashish, opium derivatives, cocaine, or amphetamine. Reports from the UN Office on Crime and Materials indicate approximately 12.7 million injectable drug users worldwide. In 2015, according to a World Health Organization (WHO) report, the deaths resulting from drug addiction were calculated to be 450000 between 15-64 years old people (Ieong, 2013).
Addiction as a brain disorder can affect people differently due to the diverse nature of substances and how harmful they are (Vahabzadeh & Ghassemi Toussi, 2016). So, the severity of addiction and its damages could vary depending on the abused substances. Craving is one of the psychological effects that drug consumers could experience and is one of the most critical issues in addiction treatment (Ieong, 2013; Sofuoglu et al., 2013). It is considered one of the main features of the substance-using disorder in the fifth edition of the diagnostic and statistical manual of mental disorders (DSM-5). It can be the anticipant of recurrence and reusing phenomenon. Although various kinds of treatments have been suggested for drug addiction, and one of the main goals of these therapies has been to reduce craving and relapse, still craving and relapse exist as the most important and common problems in the field of addiction treatment (Ieong, 2013; Sofuoglu et al., 2013).
As for all types of drug abuse, craving is the leading cause of difficulties in the treatment of the users of stimulants, including methamphetamine (Mutumba, 2021). Methamphetamine is a stimulant whose prevalence is 5.2 times higher than other substances that have destructive effects on the central nervous system (Vahabzadeh & Ghassemi Toussi, 2016). Psychological dependence is high in methamphetamine users, so its treatment gets more complicated (Cruickshank & Dyer, 2009). The principal aim of treatments is to reduce craving and relapse. The approaches include matrix therapy, cognitive rehabilitation techniques, and magnetic stimulation interventions.
Matrix therapy is an outpatient psychotherapy whose headlines are based on treating the psychiatric weaknesses of people who use stimulants. In psychotherapy sessions and individual counseling, one would believe in how drug consumption has created cognitive-behavioral problems (Eghbali et al., 2013; Hemmati Sabet et al., 2015; Seid & Dolatyari, 2015).
In cognitive rehabilitation interventions, one of the common ways is to use computer software to improve cognitive performance in problem-solving, attention, memory, and information processing speed. Apparently, these functions are severely impaired in stimulant consumers (Fals-Stewart & Lam, 2010; Ieong, 2013; Potenza et al., 2011).
Another approach in the treatment of methamphetamine dependence is to use magnetic stimulation in the brain. Repetitive transcranial magnetic stimulation (rTMS) is a noninvasive treatment intervention associated with the regular application of magnetic pulses. Various studies have been done in this field; different brain areas have been stimulated. The most affected site is the lateral-dorsal cortex of the forehead. Of course, different results have been obtained according to the stimulated hemisphere (right or left) and the used frequencies
(low frequencies, less than or equal to 1 Hz, versus higher frequencies, more than 1 Hz). Previous studies have shown the efficacy of these therapies in controlling craving and relapse (Bellamoli et al., 2014; De Sousa, 2013; Hone-Blanchet et al., 2015; Pirmoradi et al., 2013). rTMS is a new technique for treating neuropsychological disorders that cause neurobiochemical changes in the brain, and it can lead to the release of neurotransmitters involved in craving reduction, such as dopamine (Eichhammer et al., 2003).
Also, the consumption of drugs causes some neurological harm and damage (Banjara, 2015). One is the negative effect on attention (van Hemel-Ruiter et al., 2016). It has been claimed that attentional bias is involved in addiction and plays a crucial role in sustaining drug use. Attention bias means one selectively focuses on a particular environmental stimulus while neglecting other stimuli. Research suggests a bias in drug users toward drug-related stimuli and cues. Mostly, but not always, attentional bias is related to one’s motivation and purposeful behaviors. There are several ways to attenuate attention bias (Attwood et al., 2014; Barrouillet, 2011; Garland et al., 2012). One of these methods is the dot-probe task. Evidence suggests that correcting attentional bias could help treat addiction and reduce drug tendencies (Attwood et al., 2014; Barrouillet, 2011; Garland et al., 2012; Skjærvø, 2010).
Based on the above findings and the literature, these types of complementary therapies are expected to improve the symptoms of addiction and reduce the likelihood of recurrence and reuse. Thus, we can be optimistic that both therapies prevent relapse in people with the disease. The benefits of treatment should be reflected in the individual and social life of the individual, and the burden of social and economic pressures should be reduced. Therefore, the main purpose of this study is to investigate the effectiveness of these treatments to achieve these goals. On the other hand, no study has compared the effectiveness of these three therapeutic interventions or assessed changes in dopamine receptor gene expression. The present study aimed to compare the effectiveness of Matrix, rTMS, and cognitive rehabilitation interventions in reducing craving and modifying attention bias in methamphetamine users.
2. Materials and Methods
Study participants
This study was quasi-experimental with a pre-test-post-test and a 3-month follow-up design. The study participants were selected by convenient sampling from the clients of authorized drug addiction clinics in Tehran and Karaj cities, Iran, in 2019-2020. Forty-six participants were selected from outpatients addicted to methamphetamine diagnosed by a physician and or a psychologist based on standard clinical interviews. The number of participants in the study was selected according to previous research and related literature (Hyman et al., 2008; Sousa, 2013). Thus, 36 subjects were recruited and equally and randomly divided into three experimental groups: Matrix therapy, cognitive rehabilitation, and rTMS as intervention groups (12 subjects in each group). Ten other subjects were also recruited as a control group with no treatment. Six subjects (2 subjects in each group) were excluded from statistical analysis due to long absences, incomplete responses to scales, and not performing the software’s tests and evaluations. Finally, statistical analysis was performed on 40 subjects. The inclusion criteria were as follows: Being in the age range of 20 to 65 years, having a history of at least 1 year of amphetamine use, having a high score on the craving scale, and having satisfaction with participating in research. The patients were not included in the study if they were treated with non-methadone medications (such as buprenorphine, opium tincture, or sedatives to control withdrawal symptoms), had any serious psychiatric disorder, previous participation in a similar intervention program, and absence of more than two sessions from intervention therapies.
Participants were informed about the study’s aim and were instructed to sleep well and relax before each training session. We separately implemented the interventional sessions in 24 sessions for the matrix group, 15 sessions for the cognitive rehabilitation group, and 5 sessions for the rTMS candidates. We used some questionnaires as a pre-test, as demonstrated in the paragraphs below, and repeated them after the final training sessions as post-tests for all candidates.
Study instruments
All candidates were evaluated via paper- and computer-based tests as the pre-test. In both experimental and control groups, the desire for drug questionnaire (DDQ) was used as a craving assessment test. The substance dependence severity scale (SDSS) was completed to assess dependence, and dot-probe tasks (DPTs) were done to evaluate attention bias.
The dDDQ
The DDQ is used to measure instant craving. It includes three subscales: Drug use desire (7 questions), negative reinforcement (4 questions), and a distinguished control over drug use (3 questions). The range of subscales of the DDQ is from 1 to 10 (Deady, 2009; Franken et al., 2002). Internal consistencies for each factor were reported to be 0.81, 0.84, and 0.79, respectively (Franken et al., 2002). Internal consistency of DDQ has been reported as acceptable in the Iranian population (Hassani-Abharian et al., 2016).
SDSS
The SDSS is a semi-structured interview questionnaire designed based on the DSM-IV and ICD-10 drug and alcohol dependence definitions that show the intensity and frequency of the dependence over the past 30 days. The questionnaire consists of 11 questions with a maximum score of 42 (Miele, 2000). The alpha coefficient was 0.77, and the correlation between test and re-test results showed a high correlation coefficient (0.97), confirming its reliability. Construct validity was assessed by a cross-check against the general health questionnaire and the results were in favor of its validity (Motlaq et al., 2009).
DPT
We used the DPT as a pre- and post-training assessment to measure attentional bias towards stimulants’ craving-related cues. DPT is a computerized task in which two pictures appear concurrently at different locations on a computer screen. After the pictures or cues disappear, a dot appears on the monitor. Participants must respond to a feature of the probe as fast as possible. According to attentional bias to craving-related cues of the stimulant drug, the reaction to these cues is faster than that of neutral pictures, which is vice versa in normal people. When subjects selectively pay more attention to the craving-related cues, they respond quicker than neutral ones (Begh et al., 2013; De Voogd et al., 2016; Lancee et al., 2017).
Study interventions
Matrix treatment
The matrix group received twenty-four 45-minute intervention sessions (3 sessions per week). Their treatment was based on a matrix pattern. Matrix is an outpatient psychotherapy that has been introduced as a practical approach to treating stimulant users (Matrix Institute on Addictions, 2012).
Dot-probe task (DPT)
We used pictures instead of words as stimuli to make the test reasonable for patients from various educational backgrounds. For choosing the craving-related pictures of stimulant abuse, 100 craving-related pictures taken from the international affective picture system and picture collection of SINA Institute in Tehran were selected. The selected pictures were shown to 20 stimulant abusers who were not included in the main study. The abusers were said to select the most stimulant pictures based on the degree of craving they made. Then, we paired 40 target pictures with neutral ones similar in composition, size, and color. Each trial began with a 500-ms black fixation cross (8×8 mm) in a white screen center. Next, the fixation of two pictures, including a neutral one on one side and a stimulant one (craving-related picture) on the other side, was simultaneously presented for 1000 ms. After 1000 ms, the picture pair was randomly replaced with a target or dot (3 mm in diameter) either on the right or left side for 500 ms. In 50% of the trials, the target appeared in the presence of the neutral picture. The participants were asked to indicate the dot’s direction by pressing the matching button on the computer keyboard. Participants were instructed that the dot would appear in one of the two pictures’ right or left locations and were required to pay attention to the pictures and dots and perform the task as quickly and correctly as possible. In this case, both speed and accuracy were considered as essential factors. The task involved the participants in 160 dot-probe trials because each of the 40 picture pairs was displayed four times. The distance of the participants’ eyes from the screen was 50 to 70 cm. The session lasted about 5-7 min (Begh et al., 2013; De Voogd et al., 2016; Lancee et al., 2017).
Dot-probe attention bias modification training
Dot-probe training was used as an intervention for the cognitive rehabilitation group. This training task engaged the participants in 480 dot-probe trials for each session. Each of the 40 picture pairs was presented 12 times (12 ×40). Among all trials, 90% of the targets appeared at the neutral picture position and 10% at the craving-related picture position (Hakamata et al., 2010).
rTMS method
The treatment protocol included 10 sessions for each subject, performed every other day. The dorsal-lateral area of the left prefrontal cortex was the site that was repeatedly stimulated by the coil at a frequency of 10 Hz. Each session’s duration was 8 minutes, and the protocol was set out at 5 seconds of rTMS at 1200 pulses in the area. The stimulation was then stopped for 15 s (Su et al., 2017).
Data analysis
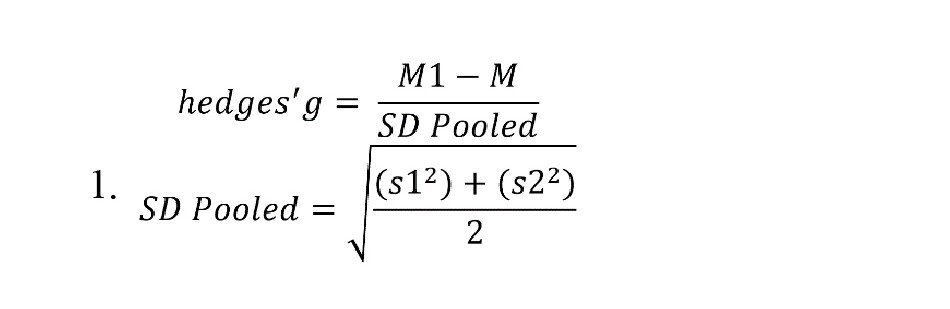
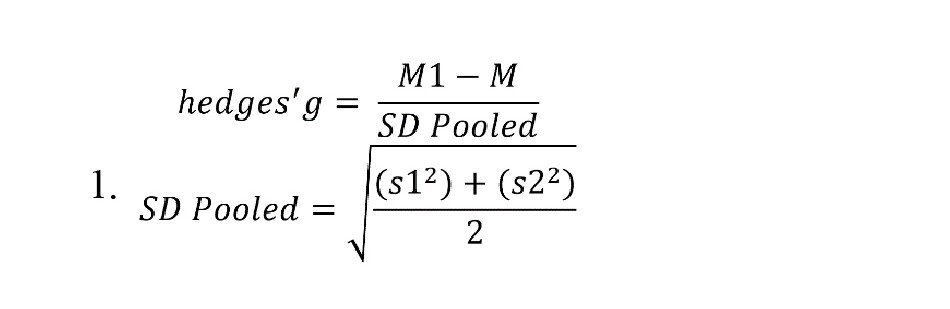
Repeated-measures analysis of variance (ANOVA) was used to evaluate and compare the effectiveness of Matrix treatment, rTMS, and cognitive intervention in the pre-test, post-test, and follow-up states. The least significant difference (LSD) post hoc test was used to compare the pairwise time steps in the dependent variables. Furthermore, due to the eta coefficient’s limitations in estimating the therapeutic effects in three different time points and pairwise comparisons, Hedges’ effect size was used more accurately to estimate the effect size. The formula for estimating the effect size of Hedges is given below (Equation 1). Due to the lack of homogeneity of the studied groups in demographic variables of age, consumption rate, and pre-test in the dependent variables, we used a one-way analysis of covariance (ANCOVA) to compare the effectiveness of different treatment methods in the dependent variables by controlling for the primary differences in pre-test craving, age, and consumption rate as covariance. P<0.05 were considered significant. Data were analyzed using SPSS software, version 23.
3. Results
The Mean±SD ages of the subjects were 38.5±6.4 years in the Matrix treatment group, 31.8±5.22 years in the cognitive modification group, 31.6±6.02 years in the rTMS group, and 31.5±5.48 years in the control group. In terms of marital status, 10% were single, 80% married, and 10% divorced in the matrix treatment group; 30% single, 60% married, and 10% divorced in the cognitive modification group; 60% single, 20% married, and 20% divorced in rTMS subjects; and 40% single, 50% married, and 10% divorced in the control group. The type of abused substance in all four groups was methamphetamine. The mean values of drug usage were 3.6 g/d in the matrix treatment group, 3.55 g/d in the cognitive modification treatment group, 4.05 g/d in the rTMS subjects, and 8 g/d in the control group. The chi-square test results showed no significant differences between the groups regarding their marital status (P>0.05). However, one-way ANOVA showed that the mean age of the matrix group was significantly higher than the cognitive modification, rTMS, and control groups (F=3.51, P=0.025).
Table 1 presents Mean±SD, and repeated measure ANOVA results to evaluate the effectiveness of matrix therapy, rTMS, and cognitive modification in reducing craving, the severity of addiction dependence, and attentional bias from pre-test to post-test and follow-up in each group.
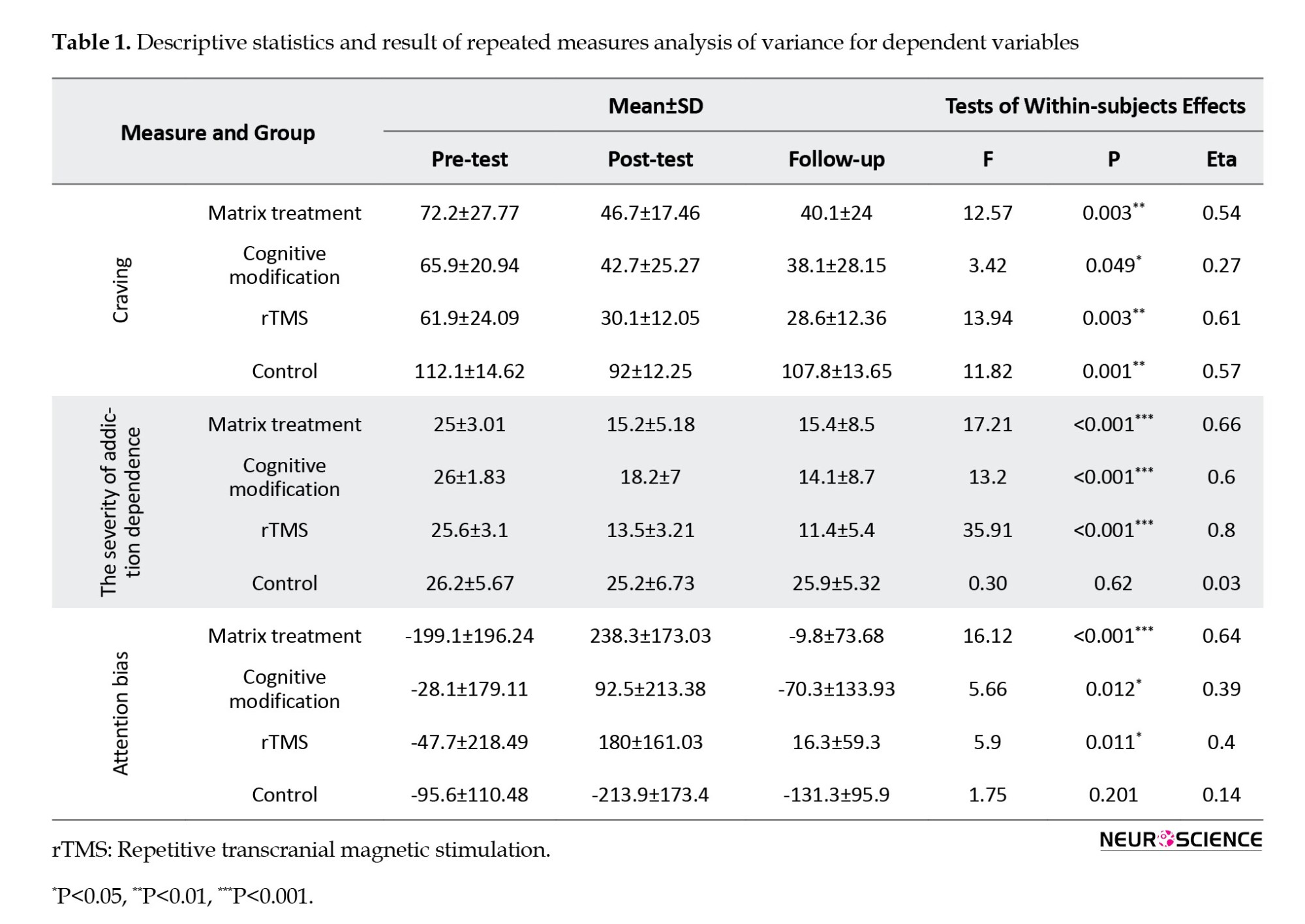
As the primary assumption of repeated measurement, Mauchly’s test of sphericity showed that the spherical hypothesis for craving variables in the matrix treatment group and cognitive modification treatment was not observed in the group’s addiction severity variable (P<0.05). Therefore, the Huynh-Feldt correction was used to interpret the assumption of homogeneity of the bias variances in the mentioned variables.
Repeated measure ANOVA results showed that the effect of time in the three stages of craving assessment was significant in all four studied groups (P<0.05). In the matrix, rTMS, and cognitive modification groups, treatment significantly affected the severity of addiction dependence and attentional bias in three assessment time points (P<0.05). In the control group, the effect of time in the three stages of assessing the severity of addiction and attention bias was not significant (P>0.05). The eta coefficient results for estimating the variation of dependent variables by different treatment conditions are also reported in Table 1.
LSD test results pairwise comparing the time steps showed a significant decrease in craving in matrix treatment, rTMS, and cognitive modification groups from pre-test to post-test and from pre-test to follow-up (P<0.01). In the control group, mean craving decreased significantly from pre-test to post-test (P<0.05). The mean severity of addiction decreased significantly from the pre-test to the post-test and from the pre-test to follow-up in the Matrix, rTMS, and cognitive modification groups (P<0.01). In the rTMS group, the mean severity of addiction significantly decreased from post-treatment to follow-up (P=0.05). The mean attentional bias in the matrix treatment group was significantly increased from pre-test to post-treatment and from pre-test to follow-up (P<0.05) and significantly decreased from post-test to follow-up (P=0.006). In the rTMS, there was a significant decrease in the time aspect of attentional bias from the post-test phase to follow-up (P=0.002). There was a significant increase from the pre-test to the post-test in the cognitive modification group and a significant decrease from the post-test to follow-up (P<0.05).
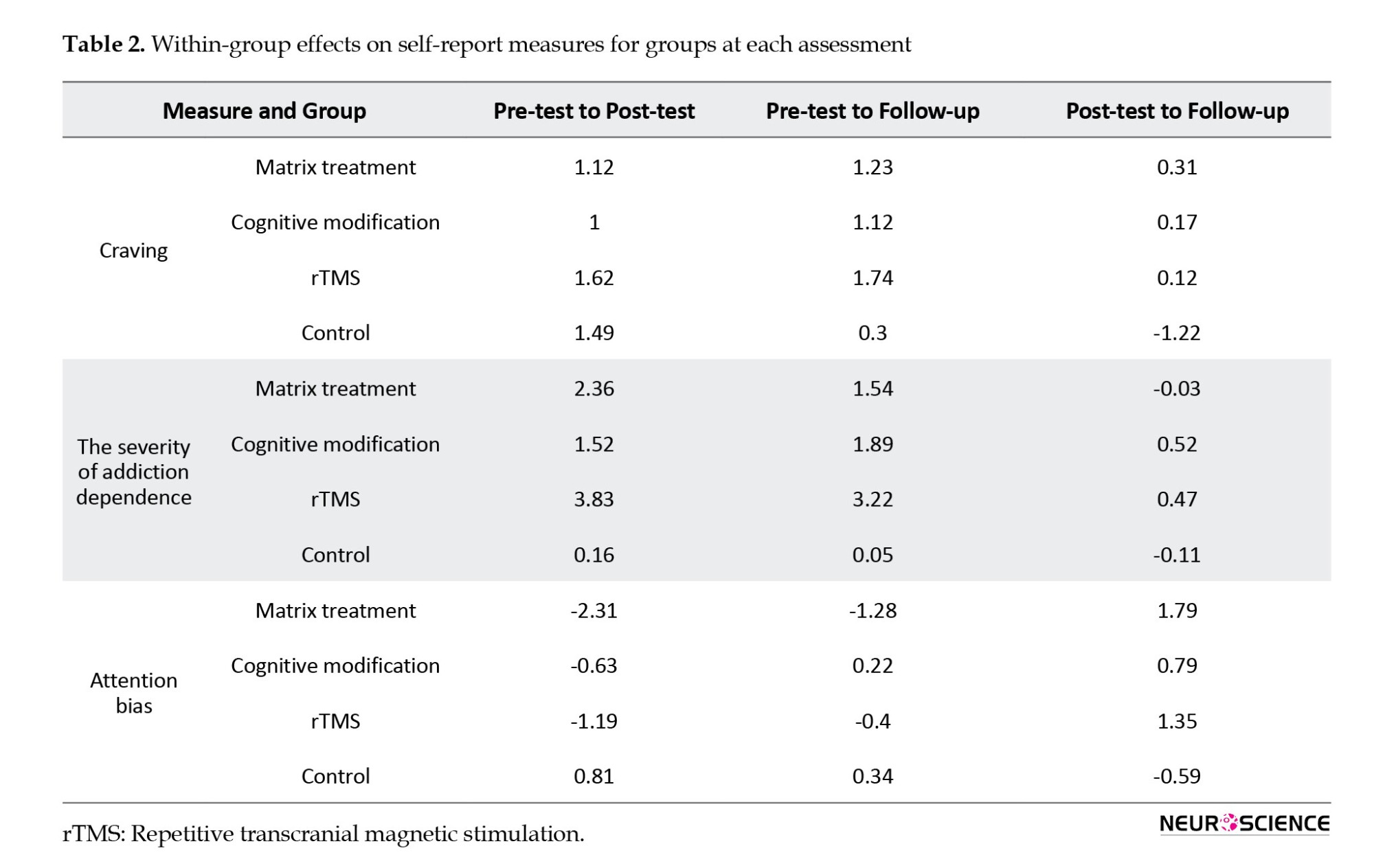
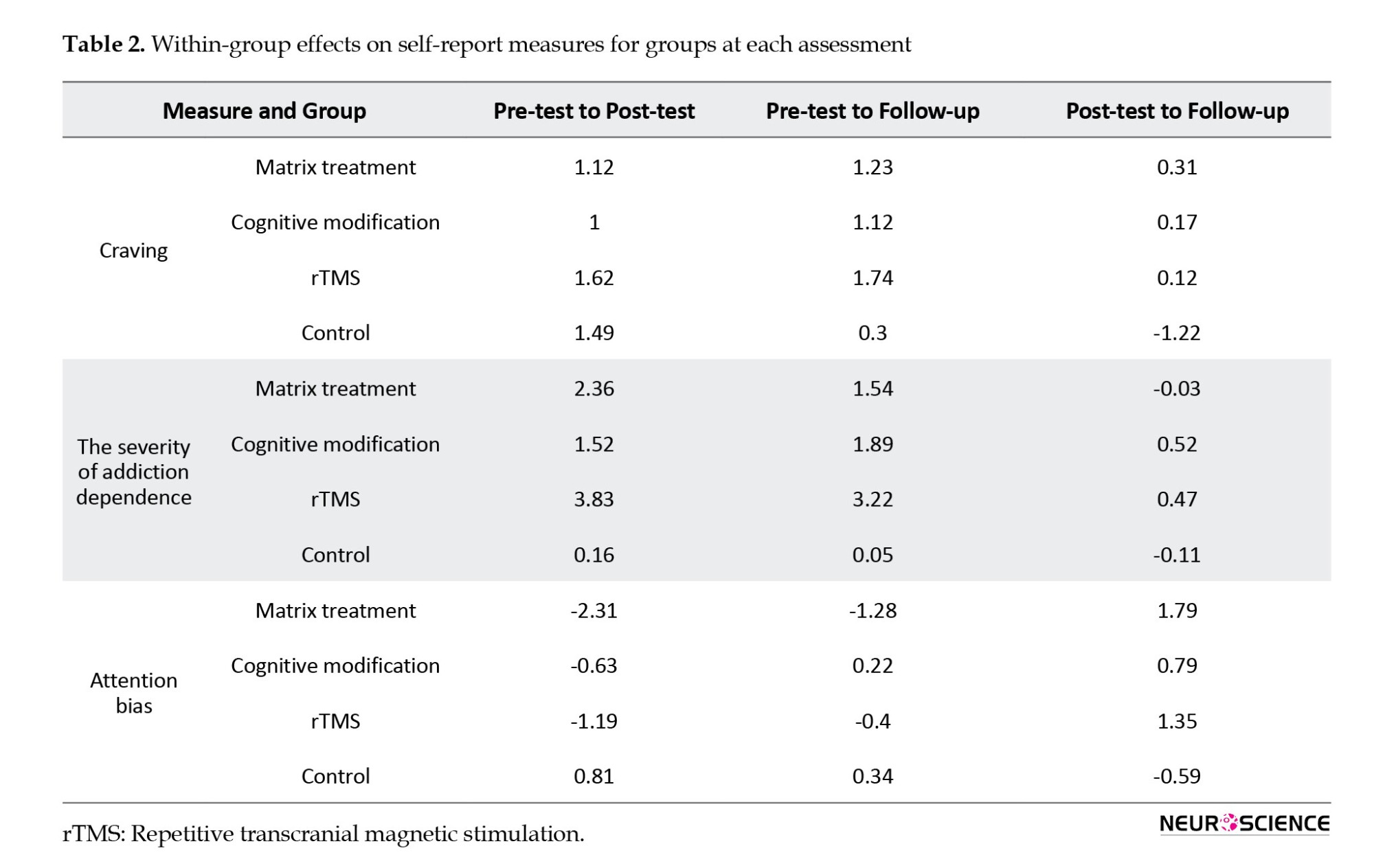
Effect sizes of standardized gain were calculated to determine the magnitude of changes during three assessment time points (Table 2). Hedges reported an effect size of 0.2, 0.5, and 0.8 as small, medium, and large, respectively.
The results of ANOVA revealed a significant difference in the pre-test craving variable (P<0.01). Due to the lack of homogeneity of the groups of study in demographic variables of age and drug consumption as well as pre-test craving variable, to compare the effectiveness of Matrix therapy, rTMS, and cognitive modification in reducing craving, the severity of the addiction, and attentional bias, we used one-way intra-group analysis of covariance (ANCOVA) to control for differences between groups in pre-test, craving, age, and consumption rate as covariates. Adjusted means and ANCOVA results are reported in Table 3.
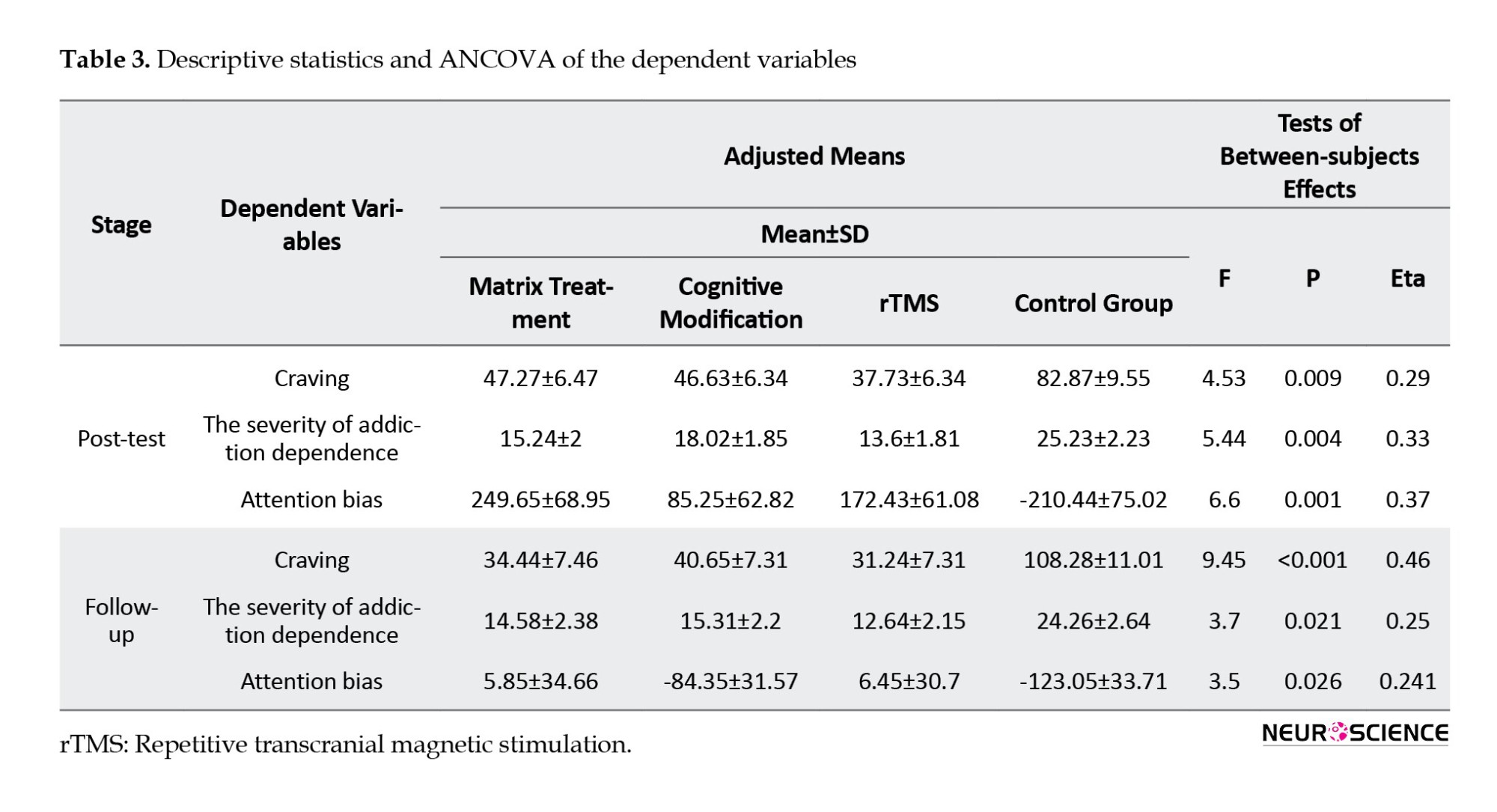
The main assumptions of ANCOVA, including the relativity of scale of dependent variables, normality of variables distribution based on the Kolmogorov-Smirnov test in studied groups (P>0.05), homogeneity of variables’ variance in studied groups based on Levene’s test (P>0.05), implementation of pre-test before treatment, the linearity of correlation between the pre-treatment and independent variables (P<0.01) and homogeneity of regression slope in the dependent variables (P>0.05) were all observed in this study. The results of ANCOVA indicated that after controlling for the effects of pre-test, age, and consumption rate as covariates, there was a significant difference between the means of the dependent variables in the study groups in both the post-test and follow-up stages (P<0.05). LSD test results by the pairwise comparison of groups revealed no significant difference between the three groups regarding the Matrix, rTMS, and cognitive modification treatment in the dependent variables in the post-test and follow-up (P>0.05). The mean value of craving, the severity of addiction dependence, and attentional bias were significantly decreased in Matrix, rTMS, and cognitive modification groups than the control group in the post-test and follow-up phases (P<0.01). The eta coefficient results are reported in Table 3 to estimate the dependent variables’ variation by the differences in the studied groups.
4. Discussion
The purpose of this study was to compare the efficacy of matrix therapy, rTMS, and cognitive modification in reducing the craving for stimulants. The effects of the matrix treatment model on amphetamine users and their craving symptoms have been studied previously. Mohammadi and Kargar Shaker, (2018) stated that 12 Matrix sessions once a week reduced methamphetamine craving and increased hardiness and psychological well-being in methamphetamine-dependent abusers. Hemmati Sabet et al., (2015) showed that this treatment could reduce methamphetamine consumption and decrease anxiety. Eghbali et al., (2013) also demonstrated that Matrix treatment could increase methadone maintenance therapy’s efficacy and reduce relapse in addicted subjects. Both studies’ results align with the data we found in the present research.
The effects of TMS on decreasing craving and attentional bias were significant during treatment and follow-up. These findings regarding craving decrease are consistent with a previous study showing a significant craving decrease after rTMS treatment in the lateral-dorsal region of the cortex (Luigjes et al., 2019; Su et al., 2020). This finding was also observed years later by studying methamphetamine users (Rostami et al., 2013). The rTMS has also been investigated in alcohol abusers, and it was found that cognitive performance improved during the executive control task, and commission error decreased. This treatment was performed in a single session in the right hemisphere’s lateral-dorsal part of the prefrontal cortex (Herremans et al., 2013). In another study conducted by Rostami and colleagues, (2013), it was shown that rTMS in methamphetamine abusers could reduce craving. Twenty subjects participated in the mentioned study. The treatment was performed in the right hemisphere in the lateral-dorsal part of the prefrontal cortex with 10 Hz and the left hemisphere in the same site with 1 Hz for 20 sessions (30 minutes each time). The results of the mentioned studies are in line with our research.
Cognitive modification therapy is a general term encompassing various techniques and methods to rehabilitate and modify neurological skills (Bowirrat et al., 2012; Campanella, 2016). It can benefit from using computerized exercises. This tool was first performed on alcohol abusers, called the alcohol avoidance method. It was found that people who performed the exercises had a lower recurrence rate than the control group after a 1-year follow-up. The study involved 509 subjects receiving cognitive-behavioral treatment. Before and after the treatment with the alcohol avoidance approach, the unconscious attention approach was measured. Half of the participants were enrolled in the experimental group, and half were in the control group. A significant decrease in recurrence was observed in the experimental group after one year of follow-up (Bickel et al., 2014).
A recent approach for the treatment and rehabilitation of substance dependents is a paper and pencil cognitive rehabilitation package called NECOREDA (neurocognitive rehabilitation for disease of addiction), which targets cognitive impairments and patients’ educational needs. The pilot study was carried out on 10 opiate- and methamphetamine-dependent patients for three months on an outpatient basis. The NECOREDA method included a series of brain exercises and tasks called “brain gym” and psycho-learning frameworks called “brain treasures” conducted in 16 training sessions followed by 16 review sessions. Due to the importance of attention disorders in these patients, 11 stages of training were focused on different types of attention, such as fixed and selective attention, split attention, and attention shift. It was found that this cognitive treatment method significantly affected the quality of the patients’ lives and effectively healed the patients and avoided substances (Rezapour et al., 2015). The results of this study are in line with the findings of our research.
Fals-Stewart & Lam, (2010) evaluated cognitive modification’s relative efficacy as a treatment for substance misuse. They selected 160 adults with substance misuse problems included in the 12-step treatment plan. They were then randomly divided into two groups. One group received standard treatment with computer-assisted typing tutorial (CATT) computerized cognitive modification (a program designed to improve cognitive performance in problem-solving, attention, memory, and information processing speed). The second group received an equally intensive attention control condition consisting of standard treatment with computer-assisted typing training (CATT). Both groups participated in 3 sessions of 50-minute weekly cognitive modification. Cognitive assessments were made at baseline, during, and immediately after the intervention, and at 3, 6, 9, and 12 months of follow-up. The results showed that those participating in the CACR program had a higher participation treatment index than the CATT group. They also had a higher commitment to treatment, with longer days remaining (129 days vs 109 days). Also, they completed the treatment more than the control group (55% vs 38%). One year later, the CACR group showed a marked improvement in assessments related to substance use and its problems, legal issues, and social-family relationships. They also spent more than 12 months without alcohol and drugs (71% vs 54%) (Fals-Stewart & Lam, 2010).
The present study used the DPT and the dot-probe training to evaluate the attentional bias to drug cues and modify this bias toward neutral stimuli for craving reduction. Attentional bias toward drug-related cues is the central cognitive aspect of addiction, which increases the impulse desire for drug use. There is considerable evidence to support this kind of cognitive bias in addicted individuals. A previous study found a significant difference in response rate to stimuli between heroin users and control individuals in terms of the accuracy of their reaction when responding to the dot-probe task (Nejati et al., 2014). The results of this study were in line with current research findings. In 2008, a dot-probe test conducted by Garousi et al. (2008) indicated a relationship between the duration of drug use and drug withdrawal and attention bias to the stimuli related to the words presented during the speech for a thousandth of a second such that with the increase in the duration of use, opioid addicts were more attentive to bias, and their reaction time was longer. Also, with increasing the duration of abandonment in individuals who have quit the drug, attention bias decreased, and their reaction time was shorter than that of the opioid-dependent group. The results of these studies are also in line with current research data.
Overall, it can be concluded that individuals involved in cognitive rehabilitation exercises participate more deeply in treatment, have more treatment reliability, and complete treatment programs better. Because of these effects, in a 1-year follow-up, they showed better results. Improvements may also be observed in areas related to one’s life.
In a randomized controlled experimental study on alcoholic addicts, the individuals were trained in 5 sessions to disengage attention from alcohol-related stimuli (attention bias modification [ABM] condition). The control group was trained on an irrelevant reaction-time (control condition) test. They measured the effects of ABM on the visual probe task. The desires for alcohol questionnaire (similar to DDQ) was employed to assess the level of craving. The follow-up data were collected up to three months after the treatment to evaluate the treatment’s overall effects and relapse times. The results illustrated that ABM effectively enabled the participants to avoid alcohol-related cues (Eberl et al., 2013).
Using the addiction severity questionnaire, we found in the present study that therapeutic approaches significantly reduced the severity of the addiction. Although data regarding the relationship between the severity of dependence and craving are limited, the current study found that treatments significantly reduced both the severity of dependence and craving. Therefore, these two features can be considered closely related.
In summary, there was no significant difference between the three groups in Matrix, rTMS, and cognitive rehabilitation treatment in the dependent variables at the post-test and follow-up stages. The mean craving, the severity of addiction dependence, and attentional bias were significantly decreased in the three groups compared to the control subjects in both the post-test and follow-up phases.
Based on this study’s findings, Matrix, cognitive rehabilitation, and rTMS treatments could significantly reduce the craving for methamphetamine use and attenuate attentional bias among patients from pre-test to post-test and follow-up. The findings of this study should be interpreted with great care. Although the researchers have attempted to control the situation as much as possible, it is difficult to control all the conditions regarding psychological treatment in all human subjects. Further studies are warranted while addressing the limitations of this study.
There are different kinds of cognitive rehabilitation training. We recommend comparing the ABM method with cognitive rehabilitation approaches such as Captains Log, online attentional bias modification, and NECOREDA. However, further studies are needed to illuminate the nature of cue-reactivity differences among those dependent on stimulant drugs such as methamphetamine. This study confirms the presence of intense cue-induced craving in response to drug use among methamphetamine addicts.
One of the limitations of this study was finding people who were only users of stimulant drugs because most people were multi-drug abusers. On the other hand, because they did not receive any medication to treat their addictive illness, there was an urgent need for continuous follow-up in the research process. Also, the lack of medication reduced subjects’ motivation to participate in the study.
In addition, the present study compared the effectiveness of treatments among male groups. Future researchers are suggested to compare the effects among female patients as well. Also, this study only used a 1-month follow-up. It would be more reliable to follow participants’ improvements in a more extended period, such as 6-12 months, and regularly track treatment effects. Further research could gather more data using more participants and more behavioral data.
Ethical Considerations
Compliance with ethical guidelines
The Vice-Chanceller of Zanjan University of Medical Sciences, approved this study (Code: ZUMS.RES.1396.96). All candidates gave their written informed consent in accordance with the research format of the Zanjan University of Medical Sciences. Ethical principles, including patient privacy and confidentiality, were respected during the study stages. Moreover, the participants were free to leave the study whenever they wished, and if desired, the research results would be available upon their request.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
References
Addiction is a recurrent and chronic brain disease. According to official UN statistics and the book of world report on drugs, addiction and its consequences and complications accounted for 183000 deaths in 2012. It is estimated that 162 to 324 million people worldwide have used at least one type of addictive drug, such as hashish, opium derivatives, cocaine, or amphetamine. Reports from the UN Office on Crime and Materials indicate approximately 12.7 million injectable drug users worldwide. In 2015, according to a World Health Organization (WHO) report, the deaths resulting from drug addiction were calculated to be 450000 between 15-64 years old people (Ieong, 2013).
Addiction as a brain disorder can affect people differently due to the diverse nature of substances and how harmful they are (Vahabzadeh & Ghassemi Toussi, 2016). So, the severity of addiction and its damages could vary depending on the abused substances. Craving is one of the psychological effects that drug consumers could experience and is one of the most critical issues in addiction treatment (Ieong, 2013; Sofuoglu et al., 2013). It is considered one of the main features of the substance-using disorder in the fifth edition of the diagnostic and statistical manual of mental disorders (DSM-5). It can be the anticipant of recurrence and reusing phenomenon. Although various kinds of treatments have been suggested for drug addiction, and one of the main goals of these therapies has been to reduce craving and relapse, still craving and relapse exist as the most important and common problems in the field of addiction treatment (Ieong, 2013; Sofuoglu et al., 2013).
As for all types of drug abuse, craving is the leading cause of difficulties in the treatment of the users of stimulants, including methamphetamine (Mutumba, 2021). Methamphetamine is a stimulant whose prevalence is 5.2 times higher than other substances that have destructive effects on the central nervous system (Vahabzadeh & Ghassemi Toussi, 2016). Psychological dependence is high in methamphetamine users, so its treatment gets more complicated (Cruickshank & Dyer, 2009). The principal aim of treatments is to reduce craving and relapse. The approaches include matrix therapy, cognitive rehabilitation techniques, and magnetic stimulation interventions.
Matrix therapy is an outpatient psychotherapy whose headlines are based on treating the psychiatric weaknesses of people who use stimulants. In psychotherapy sessions and individual counseling, one would believe in how drug consumption has created cognitive-behavioral problems (Eghbali et al., 2013; Hemmati Sabet et al., 2015; Seid & Dolatyari, 2015).
In cognitive rehabilitation interventions, one of the common ways is to use computer software to improve cognitive performance in problem-solving, attention, memory, and information processing speed. Apparently, these functions are severely impaired in stimulant consumers (Fals-Stewart & Lam, 2010; Ieong, 2013; Potenza et al., 2011).
Another approach in the treatment of methamphetamine dependence is to use magnetic stimulation in the brain. Repetitive transcranial magnetic stimulation (rTMS) is a noninvasive treatment intervention associated with the regular application of magnetic pulses. Various studies have been done in this field; different brain areas have been stimulated. The most affected site is the lateral-dorsal cortex of the forehead. Of course, different results have been obtained according to the stimulated hemisphere (right or left) and the used frequencies
(low frequencies, less than or equal to 1 Hz, versus higher frequencies, more than 1 Hz). Previous studies have shown the efficacy of these therapies in controlling craving and relapse (Bellamoli et al., 2014; De Sousa, 2013; Hone-Blanchet et al., 2015; Pirmoradi et al., 2013). rTMS is a new technique for treating neuropsychological disorders that cause neurobiochemical changes in the brain, and it can lead to the release of neurotransmitters involved in craving reduction, such as dopamine (Eichhammer et al., 2003).
Also, the consumption of drugs causes some neurological harm and damage (Banjara, 2015). One is the negative effect on attention (van Hemel-Ruiter et al., 2016). It has been claimed that attentional bias is involved in addiction and plays a crucial role in sustaining drug use. Attention bias means one selectively focuses on a particular environmental stimulus while neglecting other stimuli. Research suggests a bias in drug users toward drug-related stimuli and cues. Mostly, but not always, attentional bias is related to one’s motivation and purposeful behaviors. There are several ways to attenuate attention bias (Attwood et al., 2014; Barrouillet, 2011; Garland et al., 2012). One of these methods is the dot-probe task. Evidence suggests that correcting attentional bias could help treat addiction and reduce drug tendencies (Attwood et al., 2014; Barrouillet, 2011; Garland et al., 2012; Skjærvø, 2010).
Based on the above findings and the literature, these types of complementary therapies are expected to improve the symptoms of addiction and reduce the likelihood of recurrence and reuse. Thus, we can be optimistic that both therapies prevent relapse in people with the disease. The benefits of treatment should be reflected in the individual and social life of the individual, and the burden of social and economic pressures should be reduced. Therefore, the main purpose of this study is to investigate the effectiveness of these treatments to achieve these goals. On the other hand, no study has compared the effectiveness of these three therapeutic interventions or assessed changes in dopamine receptor gene expression. The present study aimed to compare the effectiveness of Matrix, rTMS, and cognitive rehabilitation interventions in reducing craving and modifying attention bias in methamphetamine users.
2. Materials and Methods
Study participants
This study was quasi-experimental with a pre-test-post-test and a 3-month follow-up design. The study participants were selected by convenient sampling from the clients of authorized drug addiction clinics in Tehran and Karaj cities, Iran, in 2019-2020. Forty-six participants were selected from outpatients addicted to methamphetamine diagnosed by a physician and or a psychologist based on standard clinical interviews. The number of participants in the study was selected according to previous research and related literature (Hyman et al., 2008; Sousa, 2013). Thus, 36 subjects were recruited and equally and randomly divided into three experimental groups: Matrix therapy, cognitive rehabilitation, and rTMS as intervention groups (12 subjects in each group). Ten other subjects were also recruited as a control group with no treatment. Six subjects (2 subjects in each group) were excluded from statistical analysis due to long absences, incomplete responses to scales, and not performing the software’s tests and evaluations. Finally, statistical analysis was performed on 40 subjects. The inclusion criteria were as follows: Being in the age range of 20 to 65 years, having a history of at least 1 year of amphetamine use, having a high score on the craving scale, and having satisfaction with participating in research. The patients were not included in the study if they were treated with non-methadone medications (such as buprenorphine, opium tincture, or sedatives to control withdrawal symptoms), had any serious psychiatric disorder, previous participation in a similar intervention program, and absence of more than two sessions from intervention therapies.
Participants were informed about the study’s aim and were instructed to sleep well and relax before each training session. We separately implemented the interventional sessions in 24 sessions for the matrix group, 15 sessions for the cognitive rehabilitation group, and 5 sessions for the rTMS candidates. We used some questionnaires as a pre-test, as demonstrated in the paragraphs below, and repeated them after the final training sessions as post-tests for all candidates.
Study instruments
All candidates were evaluated via paper- and computer-based tests as the pre-test. In both experimental and control groups, the desire for drug questionnaire (DDQ) was used as a craving assessment test. The substance dependence severity scale (SDSS) was completed to assess dependence, and dot-probe tasks (DPTs) were done to evaluate attention bias.
The dDDQ
The DDQ is used to measure instant craving. It includes three subscales: Drug use desire (7 questions), negative reinforcement (4 questions), and a distinguished control over drug use (3 questions). The range of subscales of the DDQ is from 1 to 10 (Deady, 2009; Franken et al., 2002). Internal consistencies for each factor were reported to be 0.81, 0.84, and 0.79, respectively (Franken et al., 2002). Internal consistency of DDQ has been reported as acceptable in the Iranian population (Hassani-Abharian et al., 2016).
SDSS
The SDSS is a semi-structured interview questionnaire designed based on the DSM-IV and ICD-10 drug and alcohol dependence definitions that show the intensity and frequency of the dependence over the past 30 days. The questionnaire consists of 11 questions with a maximum score of 42 (Miele, 2000). The alpha coefficient was 0.77, and the correlation between test and re-test results showed a high correlation coefficient (0.97), confirming its reliability. Construct validity was assessed by a cross-check against the general health questionnaire and the results were in favor of its validity (Motlaq et al., 2009).
DPT
We used the DPT as a pre- and post-training assessment to measure attentional bias towards stimulants’ craving-related cues. DPT is a computerized task in which two pictures appear concurrently at different locations on a computer screen. After the pictures or cues disappear, a dot appears on the monitor. Participants must respond to a feature of the probe as fast as possible. According to attentional bias to craving-related cues of the stimulant drug, the reaction to these cues is faster than that of neutral pictures, which is vice versa in normal people. When subjects selectively pay more attention to the craving-related cues, they respond quicker than neutral ones (Begh et al., 2013; De Voogd et al., 2016; Lancee et al., 2017).
Study interventions
Matrix treatment
The matrix group received twenty-four 45-minute intervention sessions (3 sessions per week). Their treatment was based on a matrix pattern. Matrix is an outpatient psychotherapy that has been introduced as a practical approach to treating stimulant users (Matrix Institute on Addictions, 2012).
Dot-probe task (DPT)
We used pictures instead of words as stimuli to make the test reasonable for patients from various educational backgrounds. For choosing the craving-related pictures of stimulant abuse, 100 craving-related pictures taken from the international affective picture system and picture collection of SINA Institute in Tehran were selected. The selected pictures were shown to 20 stimulant abusers who were not included in the main study. The abusers were said to select the most stimulant pictures based on the degree of craving they made. Then, we paired 40 target pictures with neutral ones similar in composition, size, and color. Each trial began with a 500-ms black fixation cross (8×8 mm) in a white screen center. Next, the fixation of two pictures, including a neutral one on one side and a stimulant one (craving-related picture) on the other side, was simultaneously presented for 1000 ms. After 1000 ms, the picture pair was randomly replaced with a target or dot (3 mm in diameter) either on the right or left side for 500 ms. In 50% of the trials, the target appeared in the presence of the neutral picture. The participants were asked to indicate the dot’s direction by pressing the matching button on the computer keyboard. Participants were instructed that the dot would appear in one of the two pictures’ right or left locations and were required to pay attention to the pictures and dots and perform the task as quickly and correctly as possible. In this case, both speed and accuracy were considered as essential factors. The task involved the participants in 160 dot-probe trials because each of the 40 picture pairs was displayed four times. The distance of the participants’ eyes from the screen was 50 to 70 cm. The session lasted about 5-7 min (Begh et al., 2013; De Voogd et al., 2016; Lancee et al., 2017).
Dot-probe attention bias modification training
Dot-probe training was used as an intervention for the cognitive rehabilitation group. This training task engaged the participants in 480 dot-probe trials for each session. Each of the 40 picture pairs was presented 12 times (12 ×40). Among all trials, 90% of the targets appeared at the neutral picture position and 10% at the craving-related picture position (Hakamata et al., 2010).
rTMS method
The treatment protocol included 10 sessions for each subject, performed every other day. The dorsal-lateral area of the left prefrontal cortex was the site that was repeatedly stimulated by the coil at a frequency of 10 Hz. Each session’s duration was 8 minutes, and the protocol was set out at 5 seconds of rTMS at 1200 pulses in the area. The stimulation was then stopped for 15 s (Su et al., 2017).
Data analysis
Repeated-measures analysis of variance (ANOVA) was used to evaluate and compare the effectiveness of Matrix treatment, rTMS, and cognitive intervention in the pre-test, post-test, and follow-up states. The least significant difference (LSD) post hoc test was used to compare the pairwise time steps in the dependent variables. Furthermore, due to the eta coefficient’s limitations in estimating the therapeutic effects in three different time points and pairwise comparisons, Hedges’ effect size was used more accurately to estimate the effect size. The formula for estimating the effect size of Hedges is given below (Equation 1). Due to the lack of homogeneity of the studied groups in demographic variables of age, consumption rate, and pre-test in the dependent variables, we used a one-way analysis of covariance (ANCOVA) to compare the effectiveness of different treatment methods in the dependent variables by controlling for the primary differences in pre-test craving, age, and consumption rate as covariance. P<0.05 were considered significant. Data were analyzed using SPSS software, version 23.
3. Results
The Mean±SD ages of the subjects were 38.5±6.4 years in the Matrix treatment group, 31.8±5.22 years in the cognitive modification group, 31.6±6.02 years in the rTMS group, and 31.5±5.48 years in the control group. In terms of marital status, 10% were single, 80% married, and 10% divorced in the matrix treatment group; 30% single, 60% married, and 10% divorced in the cognitive modification group; 60% single, 20% married, and 20% divorced in rTMS subjects; and 40% single, 50% married, and 10% divorced in the control group. The type of abused substance in all four groups was methamphetamine. The mean values of drug usage were 3.6 g/d in the matrix treatment group, 3.55 g/d in the cognitive modification treatment group, 4.05 g/d in the rTMS subjects, and 8 g/d in the control group. The chi-square test results showed no significant differences between the groups regarding their marital status (P>0.05). However, one-way ANOVA showed that the mean age of the matrix group was significantly higher than the cognitive modification, rTMS, and control groups (F=3.51, P=0.025).
Table 1 presents Mean±SD, and repeated measure ANOVA results to evaluate the effectiveness of matrix therapy, rTMS, and cognitive modification in reducing craving, the severity of addiction dependence, and attentional bias from pre-test to post-test and follow-up in each group.
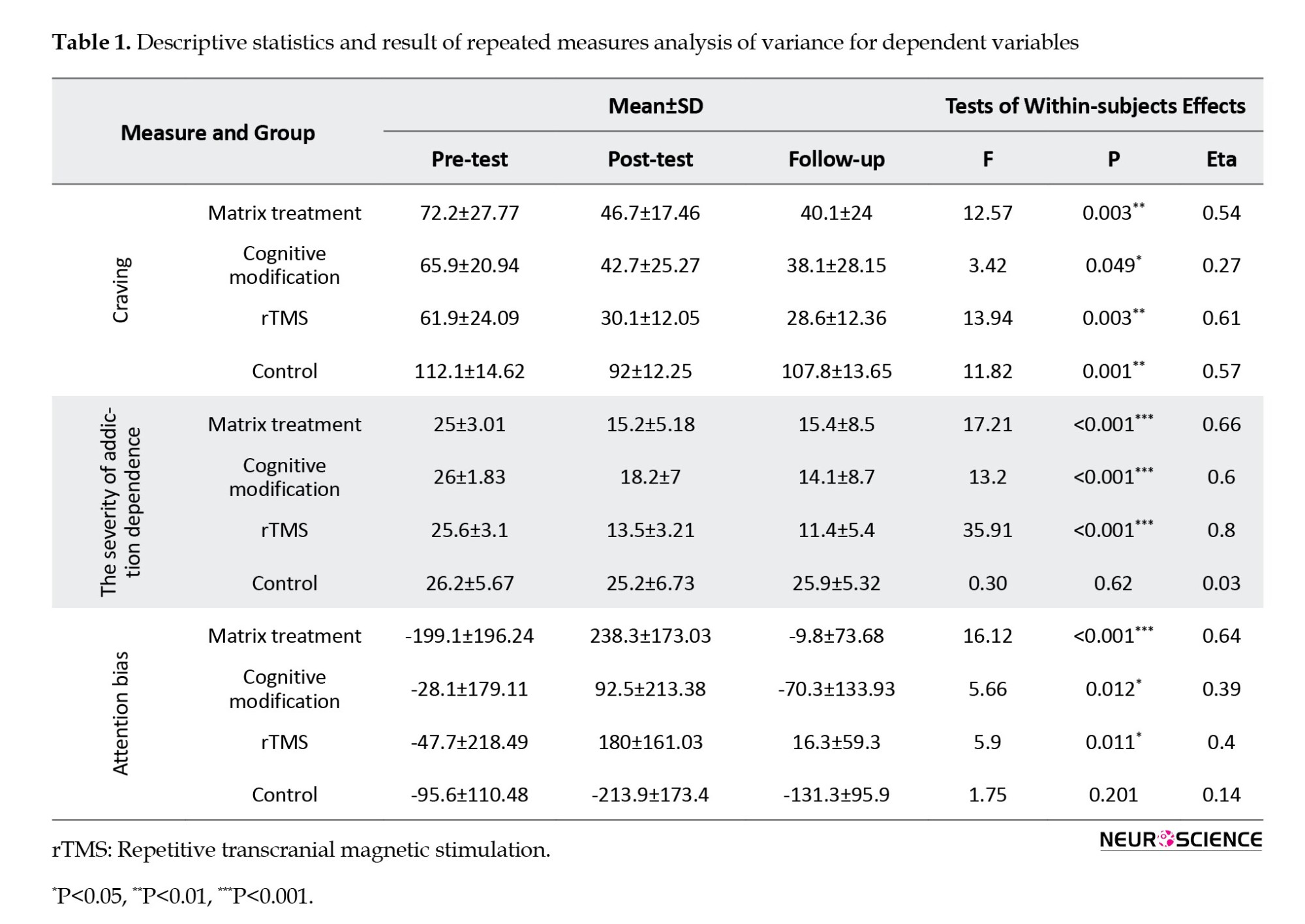
As the primary assumption of repeated measurement, Mauchly’s test of sphericity showed that the spherical hypothesis for craving variables in the matrix treatment group and cognitive modification treatment was not observed in the group’s addiction severity variable (P<0.05). Therefore, the Huynh-Feldt correction was used to interpret the assumption of homogeneity of the bias variances in the mentioned variables.
Repeated measure ANOVA results showed that the effect of time in the three stages of craving assessment was significant in all four studied groups (P<0.05). In the matrix, rTMS, and cognitive modification groups, treatment significantly affected the severity of addiction dependence and attentional bias in three assessment time points (P<0.05). In the control group, the effect of time in the three stages of assessing the severity of addiction and attention bias was not significant (P>0.05). The eta coefficient results for estimating the variation of dependent variables by different treatment conditions are also reported in Table 1.
LSD test results pairwise comparing the time steps showed a significant decrease in craving in matrix treatment, rTMS, and cognitive modification groups from pre-test to post-test and from pre-test to follow-up (P<0.01). In the control group, mean craving decreased significantly from pre-test to post-test (P<0.05). The mean severity of addiction decreased significantly from the pre-test to the post-test and from the pre-test to follow-up in the Matrix, rTMS, and cognitive modification groups (P<0.01). In the rTMS group, the mean severity of addiction significantly decreased from post-treatment to follow-up (P=0.05). The mean attentional bias in the matrix treatment group was significantly increased from pre-test to post-treatment and from pre-test to follow-up (P<0.05) and significantly decreased from post-test to follow-up (P=0.006). In the rTMS, there was a significant decrease in the time aspect of attentional bias from the post-test phase to follow-up (P=0.002). There was a significant increase from the pre-test to the post-test in the cognitive modification group and a significant decrease from the post-test to follow-up (P<0.05).
Effect sizes of standardized gain were calculated to determine the magnitude of changes during three assessment time points (Table 2). Hedges reported an effect size of 0.2, 0.5, and 0.8 as small, medium, and large, respectively.
The results of ANOVA revealed a significant difference in the pre-test craving variable (P<0.01). Due to the lack of homogeneity of the groups of study in demographic variables of age and drug consumption as well as pre-test craving variable, to compare the effectiveness of Matrix therapy, rTMS, and cognitive modification in reducing craving, the severity of the addiction, and attentional bias, we used one-way intra-group analysis of covariance (ANCOVA) to control for differences between groups in pre-test, craving, age, and consumption rate as covariates. Adjusted means and ANCOVA results are reported in Table 3.
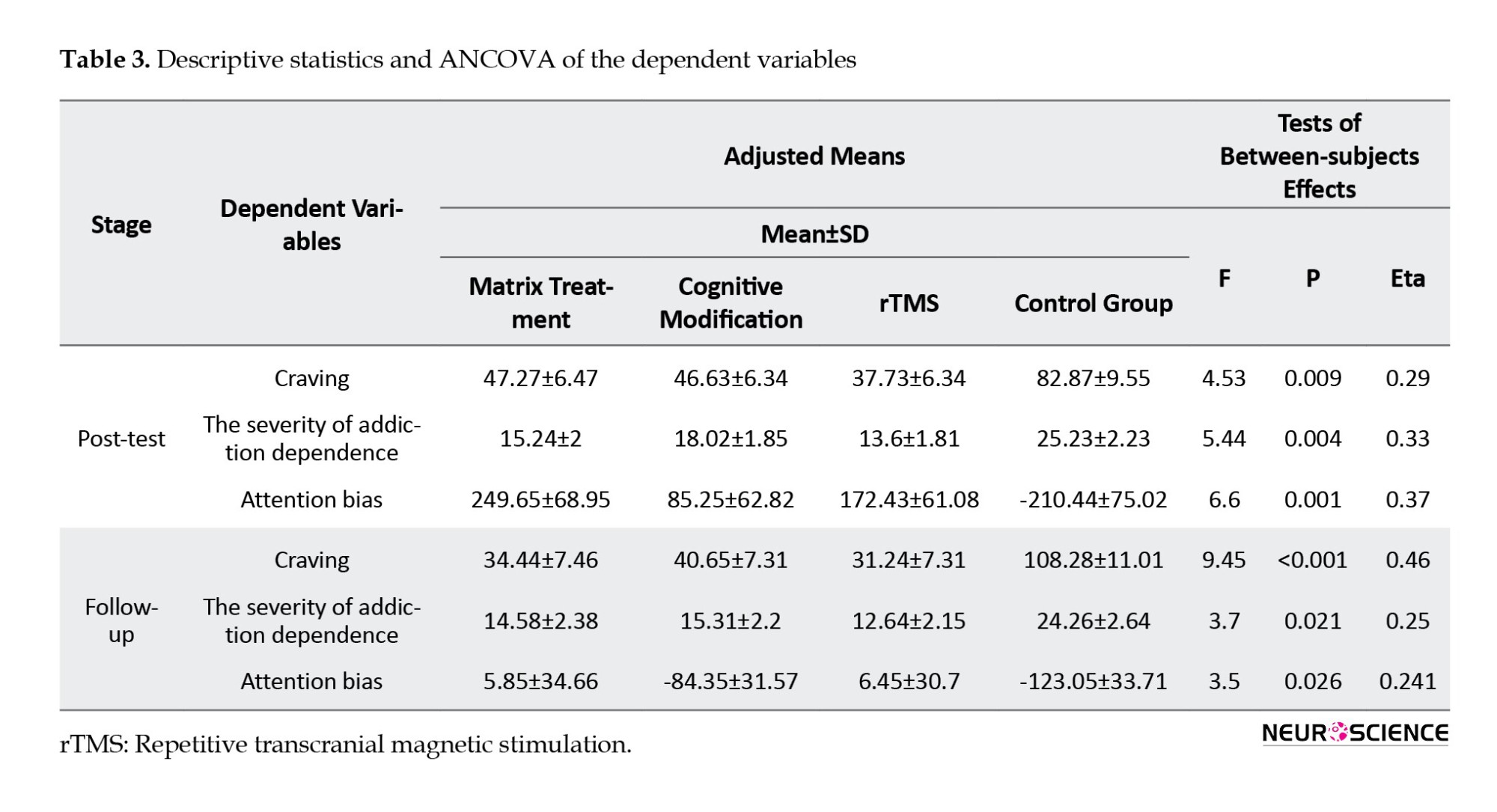
The main assumptions of ANCOVA, including the relativity of scale of dependent variables, normality of variables distribution based on the Kolmogorov-Smirnov test in studied groups (P>0.05), homogeneity of variables’ variance in studied groups based on Levene’s test (P>0.05), implementation of pre-test before treatment, the linearity of correlation between the pre-treatment and independent variables (P<0.01) and homogeneity of regression slope in the dependent variables (P>0.05) were all observed in this study. The results of ANCOVA indicated that after controlling for the effects of pre-test, age, and consumption rate as covariates, there was a significant difference between the means of the dependent variables in the study groups in both the post-test and follow-up stages (P<0.05). LSD test results by the pairwise comparison of groups revealed no significant difference between the three groups regarding the Matrix, rTMS, and cognitive modification treatment in the dependent variables in the post-test and follow-up (P>0.05). The mean value of craving, the severity of addiction dependence, and attentional bias were significantly decreased in Matrix, rTMS, and cognitive modification groups than the control group in the post-test and follow-up phases (P<0.01). The eta coefficient results are reported in Table 3 to estimate the dependent variables’ variation by the differences in the studied groups.
4. Discussion
The purpose of this study was to compare the efficacy of matrix therapy, rTMS, and cognitive modification in reducing the craving for stimulants. The effects of the matrix treatment model on amphetamine users and their craving symptoms have been studied previously. Mohammadi and Kargar Shaker, (2018) stated that 12 Matrix sessions once a week reduced methamphetamine craving and increased hardiness and psychological well-being in methamphetamine-dependent abusers. Hemmati Sabet et al., (2015) showed that this treatment could reduce methamphetamine consumption and decrease anxiety. Eghbali et al., (2013) also demonstrated that Matrix treatment could increase methadone maintenance therapy’s efficacy and reduce relapse in addicted subjects. Both studies’ results align with the data we found in the present research.
The effects of TMS on decreasing craving and attentional bias were significant during treatment and follow-up. These findings regarding craving decrease are consistent with a previous study showing a significant craving decrease after rTMS treatment in the lateral-dorsal region of the cortex (Luigjes et al., 2019; Su et al., 2020). This finding was also observed years later by studying methamphetamine users (Rostami et al., 2013). The rTMS has also been investigated in alcohol abusers, and it was found that cognitive performance improved during the executive control task, and commission error decreased. This treatment was performed in a single session in the right hemisphere’s lateral-dorsal part of the prefrontal cortex (Herremans et al., 2013). In another study conducted by Rostami and colleagues, (2013), it was shown that rTMS in methamphetamine abusers could reduce craving. Twenty subjects participated in the mentioned study. The treatment was performed in the right hemisphere in the lateral-dorsal part of the prefrontal cortex with 10 Hz and the left hemisphere in the same site with 1 Hz for 20 sessions (30 minutes each time). The results of the mentioned studies are in line with our research.
Cognitive modification therapy is a general term encompassing various techniques and methods to rehabilitate and modify neurological skills (Bowirrat et al., 2012; Campanella, 2016). It can benefit from using computerized exercises. This tool was first performed on alcohol abusers, called the alcohol avoidance method. It was found that people who performed the exercises had a lower recurrence rate than the control group after a 1-year follow-up. The study involved 509 subjects receiving cognitive-behavioral treatment. Before and after the treatment with the alcohol avoidance approach, the unconscious attention approach was measured. Half of the participants were enrolled in the experimental group, and half were in the control group. A significant decrease in recurrence was observed in the experimental group after one year of follow-up (Bickel et al., 2014).
A recent approach for the treatment and rehabilitation of substance dependents is a paper and pencil cognitive rehabilitation package called NECOREDA (neurocognitive rehabilitation for disease of addiction), which targets cognitive impairments and patients’ educational needs. The pilot study was carried out on 10 opiate- and methamphetamine-dependent patients for three months on an outpatient basis. The NECOREDA method included a series of brain exercises and tasks called “brain gym” and psycho-learning frameworks called “brain treasures” conducted in 16 training sessions followed by 16 review sessions. Due to the importance of attention disorders in these patients, 11 stages of training were focused on different types of attention, such as fixed and selective attention, split attention, and attention shift. It was found that this cognitive treatment method significantly affected the quality of the patients’ lives and effectively healed the patients and avoided substances (Rezapour et al., 2015). The results of this study are in line with the findings of our research.
Fals-Stewart & Lam, (2010) evaluated cognitive modification’s relative efficacy as a treatment for substance misuse. They selected 160 adults with substance misuse problems included in the 12-step treatment plan. They were then randomly divided into two groups. One group received standard treatment with computer-assisted typing tutorial (CATT) computerized cognitive modification (a program designed to improve cognitive performance in problem-solving, attention, memory, and information processing speed). The second group received an equally intensive attention control condition consisting of standard treatment with computer-assisted typing training (CATT). Both groups participated in 3 sessions of 50-minute weekly cognitive modification. Cognitive assessments were made at baseline, during, and immediately after the intervention, and at 3, 6, 9, and 12 months of follow-up. The results showed that those participating in the CACR program had a higher participation treatment index than the CATT group. They also had a higher commitment to treatment, with longer days remaining (129 days vs 109 days). Also, they completed the treatment more than the control group (55% vs 38%). One year later, the CACR group showed a marked improvement in assessments related to substance use and its problems, legal issues, and social-family relationships. They also spent more than 12 months without alcohol and drugs (71% vs 54%) (Fals-Stewart & Lam, 2010).
The present study used the DPT and the dot-probe training to evaluate the attentional bias to drug cues and modify this bias toward neutral stimuli for craving reduction. Attentional bias toward drug-related cues is the central cognitive aspect of addiction, which increases the impulse desire for drug use. There is considerable evidence to support this kind of cognitive bias in addicted individuals. A previous study found a significant difference in response rate to stimuli between heroin users and control individuals in terms of the accuracy of their reaction when responding to the dot-probe task (Nejati et al., 2014). The results of this study were in line with current research findings. In 2008, a dot-probe test conducted by Garousi et al. (2008) indicated a relationship between the duration of drug use and drug withdrawal and attention bias to the stimuli related to the words presented during the speech for a thousandth of a second such that with the increase in the duration of use, opioid addicts were more attentive to bias, and their reaction time was longer. Also, with increasing the duration of abandonment in individuals who have quit the drug, attention bias decreased, and their reaction time was shorter than that of the opioid-dependent group. The results of these studies are also in line with current research data.
Overall, it can be concluded that individuals involved in cognitive rehabilitation exercises participate more deeply in treatment, have more treatment reliability, and complete treatment programs better. Because of these effects, in a 1-year follow-up, they showed better results. Improvements may also be observed in areas related to one’s life.
In a randomized controlled experimental study on alcoholic addicts, the individuals were trained in 5 sessions to disengage attention from alcohol-related stimuli (attention bias modification [ABM] condition). The control group was trained on an irrelevant reaction-time (control condition) test. They measured the effects of ABM on the visual probe task. The desires for alcohol questionnaire (similar to DDQ) was employed to assess the level of craving. The follow-up data were collected up to three months after the treatment to evaluate the treatment’s overall effects and relapse times. The results illustrated that ABM effectively enabled the participants to avoid alcohol-related cues (Eberl et al., 2013).
Using the addiction severity questionnaire, we found in the present study that therapeutic approaches significantly reduced the severity of the addiction. Although data regarding the relationship between the severity of dependence and craving are limited, the current study found that treatments significantly reduced both the severity of dependence and craving. Therefore, these two features can be considered closely related.
In summary, there was no significant difference between the three groups in Matrix, rTMS, and cognitive rehabilitation treatment in the dependent variables at the post-test and follow-up stages. The mean craving, the severity of addiction dependence, and attentional bias were significantly decreased in the three groups compared to the control subjects in both the post-test and follow-up phases.
Based on this study’s findings, Matrix, cognitive rehabilitation, and rTMS treatments could significantly reduce the craving for methamphetamine use and attenuate attentional bias among patients from pre-test to post-test and follow-up. The findings of this study should be interpreted with great care. Although the researchers have attempted to control the situation as much as possible, it is difficult to control all the conditions regarding psychological treatment in all human subjects. Further studies are warranted while addressing the limitations of this study.
There are different kinds of cognitive rehabilitation training. We recommend comparing the ABM method with cognitive rehabilitation approaches such as Captains Log, online attentional bias modification, and NECOREDA. However, further studies are needed to illuminate the nature of cue-reactivity differences among those dependent on stimulant drugs such as methamphetamine. This study confirms the presence of intense cue-induced craving in response to drug use among methamphetamine addicts.
One of the limitations of this study was finding people who were only users of stimulant drugs because most people were multi-drug abusers. On the other hand, because they did not receive any medication to treat their addictive illness, there was an urgent need for continuous follow-up in the research process. Also, the lack of medication reduced subjects’ motivation to participate in the study.
In addition, the present study compared the effectiveness of treatments among male groups. Future researchers are suggested to compare the effects among female patients as well. Also, this study only used a 1-month follow-up. It would be more reliable to follow participants’ improvements in a more extended period, such as 6-12 months, and regularly track treatment effects. Further research could gather more data using more participants and more behavioral data.
Ethical Considerations
Compliance with ethical guidelines
The Vice-Chanceller of Zanjan University of Medical Sciences, approved this study (Code: ZUMS.RES.1396.96). All candidates gave their written informed consent in accordance with the research format of the Zanjan University of Medical Sciences. Ethical principles, including patient privacy and confidentiality, were respected during the study stages. Moreover, the participants were free to leave the study whenever they wished, and if desired, the research results would be available upon their request.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
References
Hassani-Abharian, P., Mokri, A., Ganjgahi, H., Oghabian, M. A., & Ekhtiari, H. (2016). Validation for Persian versions of “desire for drug questionnaire” and “obsessive compulsive drug use scale” in heroin dependents. Archives of Iranian Medicine, 19(9), 659-665. [PMID]
Attwood, A. S., Williams, T., Adams, S., McClernon, F. J., & Munafò, M. R. (2014). Effects of varenicline and cognitive bias modification on neural response to smoking-related cues: study protocol for a randomized controlled study. Trials, 15, 391. [DOI:10.1186/1745-6215-15-391] [PMID]
Banjara, M. (2015). Marijuana: Neurotoxic or neuroprotective? Global Journal of Medical Research, 15, 7-10. [Link]
Barrouillet, P. (2011). Dual-process theories and cognitive development: Advances and challenges. Developmental Review, 31(2-3), 79-85. [DOI:10.1016/j.dr.2011.07.002]
Begh, R., Munafò, M. R., Shiffman, S., Ferguson, S. G., Nichols, L., & Mohammed, M. A., et al. (2013). Attentional bias retraining in cigarette smokers attempting smoking cessation (ARTS): Study protocol for a double blind randomized controlled trial. BMC Public Health, 13, 1176. [DOI:10.1186/1471-2458-13-1176] [PMID]
Bellamoli, E., Manganotti, P., Schwartz, R. P., Rimondo, C., Gomma, M., & Serpelloni, G. (2014). rTMS in the treatment of drug addiction: An update about human studies. Behavioral Neurology, 2014, 815215. [DOI:10.1155/2014/815215] [PMID]
Bickel, W. K., Moody, L., & Quisenberry, A. (2014). Computerized working-memory training as a candidate adjunctive treatment for addiction. Alcohol Research: Current Reviews, 36(1), 123-126. [PMID]
Bowirrat, A., Chen, T. J., Oscar-Berman, M., Madigan, M., Chen, A. L., & Bailey, J. A., et al. (2012). Neuropsychopharmacology and neurogenetic aspects of executive functioning: should reward gene polymorphisms constitute a diagnostic tool to identify individuals at risk for impaired judgment? Molecular Neurobiology, 45(2), 298-313. [DOI:10.1007/s12035-012-8247-z] [PMID]
Campanella, S. (2016). Neurocognitive rehabilitation for addiction medicine: from neurophysiological markers to cognitive rehabilitation and relapse prevention. Progress in Brain Research, 224, 85–103. [DOI:10.1016/bs.pbr.2015.07.014] [PMID]
Cruickshank, C. C., & Dyer, K. R. (2009). A review of the clinical pharmacology of methamphetamine. Addiction, 104(7), 1085-1099. [DOI:10.1111/j.1360-0443.2009.02564.x] [PMID]
De Sousa, A. (2013). Repetitive transcranial magnetic stimulation (rTMS) in the management of alcohol dependence and other substance abuse disorders-emerging data and clinical relevance. Basic and Clinical Neuroscience, 4(3), 271-275. [PMID]
De Voogd, E., Wiers, R., Prins, P., De Jong, P., Boendermaker, W., & Zwitser, R., et al. (2016). Online attentional bias modification training targeting anxiety and depression in unselected adolescents: Short-and long-term effects of a randomized controlled trial. Behaviour Research and Therapy, 87, 11-22. [DOI:10.1016/j.brat.2016.08.018] [PMID]
Deady, M. (2009). A review of screening, assessment and outcome measures for drug and alcohol settings. Drug and Alcohol and Mental Health Information Management Project. NADA – The Network of Alcohol and other Drugs Agencies. [Link]
Eberl, C., Wiers, R. W., Pawelczack, S., Rinck, M., Becker, E. S., & Lindenmeyer, J. (2013). Approach bias modification in alcohol dependence: do clinical effects replicate and for whom does it work best? Developmental Cognitive Neuroscience, 4, 38-51. [DOI:10.1016/j.dcn.2012.11.002] [PMID]
Eghbali, H., Zare, M., Bakhtiari, A., Monirpoor, N., & Ganjali, A. (2013). The effectiveness of matrix interventions in improving methadone treatment. International Journal of High Risk Behaviors & Addiction, 1(4), 159-165. [DOI:10.5812/ijhrba.7906]
Eichhammer, P., Johann, M., Kharraz, A., Binder, H., Pittrow, D., Wodarz, N., & Hajak, G. (2003). High-frequency repetitive transcranial magnetic stimulation decreases cigarette smoking. The Journal of clinical psychiatry, 64(8), 951–953. [DOI: 10.4088/jcp.v64n0815]
Fals-Stewart, W., & Lam, W. K. (2010). Computer-assisted cognitive rehabilitation for the treatment of patients with substance use disorders: A randomized clinical trial. Experimental and Clinical Psychopharmacology, 18(1), 87-98. [DOI:10.1037/a0018058] [PMID]
Franken, I. H., Hendriksa, V. M., & van den Brink, W. (2002). Initial validation of two opiate craving questionnaires: the Obsessive Compulsive Drug Use Scale and the Desires for Drug Questionnaire. Addictive Behaviors, 27(5), 675-685. [DOI:10.1016/S0306-4603(01)00201-5] [PMID]
Garland, E. L., Boettiger, C. A., Gaylord, S., Chanon, V. W., & Howard, M. O. (2012). Mindfulness is inversely associated with alcohol attentional bias among recovering alcohol-dependent adults. Cognitive Therapy and Research, 36(5), 441-450. [DOI:10.1007/s10608-011-9378-7] [PMID]
Garousi, M., Majid, F., Kiomars, M., & Ghajour, A. (2008). Investigating the relationship between drug use and withdrawal in attentional bias to opiate-related sedative stimuli. Quarterly Journal of Psychology University of Tabriz, 4(15), 153-173.
Hakamata, Y., Lissek, S., Bar-Haim, Y., Britton, J. C., Fox, N. A., & Leibenluft, E., et al. (2010). Attention bias modification treatment: a meta-analysis toward the establishment of novel treatment for anxiety. Biological Psychiatry, 68(11), 982-990. [DOI:10.1016/j.biopsych.2010.07.021] [PMID]
Hemmati Sabet, A., Hemmati, M., Poustchi, M., Nejad Hashem, M., Haghighi, M., & Ahmadpanah, M. (2015). The effect of matrix method on anxiety and attitude toward methamphetamine and crack abuse in males referring to addiction treatment centers in tonkabon, Iran. Avicenna Journal of Neuro Psycho Physiology, 2(4), 88-92. [Link]
Herremans, S. C., Vanderhasselt, M. A., De Raedt, R., & Baeken, C. (2013). Reduced intra-individual reaction time variability during a go-NoGo task in detoxified alcohol-dependent patients after one right-sided dorsolateral prefrontal HF-rTMS session. Alcohol and Alcoholism, 48(5), 552-557. [DOI:10.1093/alcalc/agt054] [PMID]
Hone-Blanchet, A., Ciraulo, D. A., Pascual-Leone, A., & Fecteau, S. (2015). Noninvasive brain stimulation to suppress craving in substance use disorders: Review of human evidence and methodological considerations for future work. Neuroscience & Biobehavioral Reviews, 59, 184-200. [DOI:10.1016/j.neubiorev.2015.10.001] [PMID]
Hyman, S. M., Paliwal, P., Chaplin, T.M., Mazure, C.M., Rounsaville, B. J., & Sinha, R. (2008). Severity of childhood trauma is predictive of cocaine relapse outcomes in women but not men. Drug & Alcohol Dependence, 92(1-3), 208-216. [DOI:10.1016/j.drugalcdep.2007.08.006] [PMID]
Ieong, H. F. H. (2013). Literature review craving: The neurotoxic and social-cognitive effects of drugs consumptions of adults, adolescences, including prenatal exposure to drugs of abuse. Paper presented at: Proceedings of the 8th Mainland, Hong Kong and Macau Conference on Prevention of Drug Abuse (Macau). [Link]
Lancee, J., Yasiney, S. L., Brendel, R. S., Boffo, M., Clarke, P. J. F., & Salemink, E. (2017). Attentional bias modification training for insomnia: A double-blind placebo controlled randomized trial. Plos One, 12(4), e0174531. [DOI:10.1371/journal.pone.0174531] [PMID]
Luigjes, J., Segrave, R., de Joode, N., Figee, M., & Denys, D. (2019). Efficacy of invasive and noninvasive brain modulation interventions for addiction. Neuropsychology Review, 29(1), 116-138. [DOI:10.1007/s11065-018-9393-5] [PMID]
Substance Abuse and Mental Health Services Administration. Counselor’s treatment manual: Matrix intensive outpatient treatment for people with stimulant use disorders. Maryland: Substance Abuse and Mental Health Services Administration; 2013. [Link]
Miele, G. M., Carpenter, K. M., Smith Cockerham, M., Dietz Trautman, K., Blaine, J., & Hasin, D. S. (2000). Concurrent and predictive validity of the Substance Dependence Severity Scale (SDSS). Drug and Alcohol Dependence, 59(1), 77–88. [DOI:10.1016/S0376-8716(99)00110-6] [PMID]
Mohammadi, A., & Kargar Shaker, A. (2018). [Effectiveness of structured matrix treatment on craving, hardiness and well-being in methamphetamine abusers (Persian)]. Journal of Police Medicine, 7(2), 75-80. [DOI:10.30505/7.2.75]
Motlaq, M. E., Garrusi, B., & Shamsinejad, B. (2009). Reliability and validity of a Persian version of Substance Dependence Severity Scale (SDSS). Addiction & Health, 1(2), 87–91. [PMID]
Mutumba, M., Moskowitz, J. T., Neilands, T. B., Lee, J. Y., Dilworth, S. E., & Carrico, A. W. (2021). A mindfulness-based, stress and coping model of craving in methamphetamine users. Plos One, 16(5), e0249489. [DOI:10.1371/journal.pone.0249489] [PMID]
Nejati, V., Sadeghi Meresht, A., Moradi, Y., & Barzegar, B. (2014). The influence of consciousness on inhibition of and attentional bias to stimuli associated with drugs among heroin users. Research on Addiction, 8(30), 21-34. [Link]
Pirmoradi, M., Dolatshahi, B., Rostami, R., Mohammadkhani, P., & Dadkhah, A. (2013). Effect of repetitive transcranial magnetic stimulation (rTMS) in reducing severity of the signs and symptoms, such as cognitive, bodily and negativity-worthlessness of depression in patients with recurrent major depression disorder. Journal of Ardabil University of Medical Sciences, 13(2), 174-186. [Link]
Potenza, M. N., Sofuoglu, M., Carroll, K. M., & Rounsaville, B. J. (2011). Neuroscience of behavioral and pharmacological treatments for addictions. Neuron, 69(4), 695-712. [DOI:10.1016/j.neuron.2011.02.009] [PMID]
Rezapour, T., Hatami, J., Farhoudian, A., Sofuoglu, M., Noroozi, A., & Daneshmand, R., et al. (2015). NEuro cognitive rehabilitation for disease of addiction (NECOREDA) program: From development to trial. Basic and Clinical Neuroscience, 6(4), 291-298. [PMID]
Rostami, R., Kenari, A. H., Mirzaieyan, B., & Kochaksaraie, M. (2012). [The efficacy of repeated transcranial magnetic stimulation of the brain on the rate of material craving in addicts to methamphetaime (Persian)]. Journal of Mazandaran University of Medical Sciences, 22 (1),164-176. [Link]
Seid, S. H., & Dolatyari, N. (2015). The impact of matrix treatment (family training) in reducing the amount of drug consumption in heroin and crack addicts. Health, 7(04), 419. [DOI:10.4236/health.2015.74048]
Skjærvø, I. (2010). Attentional bias towards supraliminal and subliminal smoking cues in smokers: Effects of cognitive load on attentional bias [MA thesis]. Oslo: Norwegian Centre for Violence and Traumatic Stress Studies. [Link]
Sofuoglu, M., DeVito, E. E., Waters, A. J., & Carroll, K. M. (2013).Cognitive enhancement as a treatment for drug addictions. Neuropharmacology, 64(1), 452–463. [DOI:10.1016/j.neuropharm.2012.06.021] [PMID]
Sousa, A.D. (2013). Repetitive Transcranial Magnetic Stimulation (rTMS) in the management of alcohol dependence and other substance abuse disorders - emerging data and clinical relevancebasic. Clinical Neuroscience, 4(3), 271-275. [PMID]
Su, H., Liu, Y., Yin, D., Chen, T., Li, X., & Zhong, N., et al. (2020). Neuroplastic changes in resting-state functional connectivity after rTMS intervention for methamphetamine craving. Neuropharmacology, 175, 108177. [DOI:10.1016/j.neuropharm.2020.108177] [PMID]
Su, H., Zhong, N., Gan, H., Wang, J., Han, H., & Chen, T., et al. (2017). High frequency repetitive transcranial magnetic stimulation of the left dorsolateral prefrontal cortex for methamphetamine use disorders: A randomized clinical trial. Drug and Alcohol Dependence, 175, 84-91. [DOI:10.1016/j.drugalcdep.2017.01.037] [PMID]
Type of Study: Original |
Subject:
Cognitive Neuroscience
Received: 2021/02/4 | Accepted: 2021/07/24 | Published: 2024/11/1
Received: 2021/02/4 | Accepted: 2021/07/24 | Published: 2024/11/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |