Volume 16, Issue 4 (July & August 2025)
BCN 2025, 16(4): 763-776 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Parsa M, Abdollahi I, Negahban H, Sanjari M A, Bakhshi E, Haddadiyan H F. Reliability of Center of Pressure Measures in Chronic Stroke Survivors: Influence of Motor and Cognitive Dual-tasking. BCN 2025; 16 (4) :763-776
URL: http://bcn.iums.ac.ir/article-1-3037-en.html
URL: http://bcn.iums.ac.ir/article-1-3037-en.html
Mitra Parsa1 

 , Iraj Abdollahi *1
, Iraj Abdollahi *1 

 , Hossein Negahban2
, Hossein Negahban2 

 , Mohammad Ali Sanjari3
, Mohammad Ali Sanjari3 

 , Enayatollah Bakhshi4
, Enayatollah Bakhshi4 

 , Haniyeh Fakur Haddadiyan5
, Haniyeh Fakur Haddadiyan5 




 , Iraj Abdollahi *1
, Iraj Abdollahi *1 

 , Hossein Negahban2
, Hossein Negahban2 

 , Mohammad Ali Sanjari3
, Mohammad Ali Sanjari3 

 , Enayatollah Bakhshi4
, Enayatollah Bakhshi4 

 , Haniyeh Fakur Haddadiyan5
, Haniyeh Fakur Haddadiyan5 


1- Neuromusculoskeletal Rehabilitation Research Center, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Department of Physiotherapy, School of Paramedical and Rehabilitation Sciences, Mashhad University of Medical Sciences, Mashhad, Iran. & Orthopedic Research Center, Mashhad University of Medical Sciences, Mashhad, Iran.
3- Department of Basic Rehabilitation Sciences, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran.
4- Department of Biostatistics and Epidemiology, School of Social Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
5- Department of Physiotherapy, School of Paramedical and Rehabilitation Sciences, Mashhad University of Medical Sciences, Mashhad, Iran.
2- Department of Physiotherapy, School of Paramedical and Rehabilitation Sciences, Mashhad University of Medical Sciences, Mashhad, Iran. & Orthopedic Research Center, Mashhad University of Medical Sciences, Mashhad, Iran.
3- Department of Basic Rehabilitation Sciences, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran.
4- Department of Biostatistics and Epidemiology, School of Social Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
5- Department of Physiotherapy, School of Paramedical and Rehabilitation Sciences, Mashhad University of Medical Sciences, Mashhad, Iran.
Full-Text [PDF 623 kb]
| Abstract (HTML)
Full-Text:
1. Introduction
Approximately 50% of stroke survivors experience residual physical disabilities (Corriveau et al., 2004; Sawacha et al., 2013), leading to deficits in sensory, musculoskeletal, perceptual, and cognitive systems, affecting balance control and finally increasing the risk of falls (Corriveau et al., 2004; Jagroop et al., 2023; Sawacha et al., 2013). Therefore, the primary goal of stroke rehabilitation is to enhance balance control, requiring reliable balance measures to guide rehabilitation and monitor progress over time (Jette et al, 2009; Mansfield & Inness, 2015). Clinical balance scales fail to reveal underlying dyscontrol, which could potentially increase the risk of falling as the compensatory strategies used to complete tasks remain unknown (Mansfield & Inness, 2015).
The solution could be to record the center of pressure (CoP) excursion using a force platform in a laboratory setting (Jette et al., 2009; Sackley, 1991; Sawacha et al., 2013). CoP parameters can differentiate between fallers and non-fallers (Melzer et al., 2004; Melzeret al., 2010; Pajala et al., 2008) and are associated with clinical outcome measures in elderly and post-stroke individuals (Sawacha et al., 2013), but the intrinsic variability of CoP measures influences their reliability in postural control assessments. Additionally, reliability is not a static characteristic and varies based on the population (Gasq et al., 2014; Lafond et al., 2004).
To date, several studies have demonstrated acceptable CoP measures reliability in assessing balance in populations with disequilibrium problems (Mohammadi-Rad et al., 2022; Ruhe et al., 2010; Salavati et al., 2009; Terra et al., 2020), healthy elders (Lin et al., 2008; Moghadam et al., 2011; Salehi et al., 2010), and young adults (Fullin et al., 2022; Lo et al., 2022). Few studies have reported it throughout various stages of post-stroke recovery (Bower et al., 2014; Gasq et al., 2014; Gray et al., 2014; Martello et al., 2017). It is worth noting that only one study has specifically examined the reliability of CoP-based variables among chronic stroke survivors, in which a limited number of conventional variables were selected as a part of the main objective (Jagroop et al., 2023). However, during the chronic stage of stroke recovery, rehabilitative interventions have a significant net effect on the patient’s improvement, as spontaneous brain recovery has almost plateaued (Bernhardt et al., 2017). Accordingly, assessing the reliability of CoP measures in the chronic stage of stroke recovery could provide deeper insights into clinical decision-making and upcoming research.
Individuals have limited cognitive capacity based on the attentional capacity theory (Kahya et al., 2019), so they cannot perform two simultaneous tasks efficiently, known as the dual-task effect (Arpaia et al., 2024). Research has indicated that older adults and individuals with age-related neurodegenerative conditions experience higher costs of dual-tasking (Kahya et al., 2019). This condition leads to an elevated risk of falls and loss of independence (Arpaia et al., 2024; Kahya et al., 2019), particularly in post-stroke individuals compared to healthy adults (Tisserand et al., 2018). It is notable that dual-tasking also leads to spatiotemporal locomotor adaptations, which may help post-stroke individuals maintain their balance during dual-task conditions (Ghai et al., 2017; Tisserand et al., 2018). Consequently, monitoring the balance control system during dual-tasking could be beneficial for a more accurate impairment diagnosis and tracking of rehabilitation outcomes. So far, a study has examined the reliability of CoP measures during different postural stability tasks in post-stroke patients, regardless of the influence of dual-tasking on CoP measures reliability (Gray et al., 2014). Therefore, in this study, we investigated the reliability of CoP measures under various dual-task conditions.
Moreover, the reliability of CoP measures in tandem standing in post-stroke individuals has not been studied. However, this narrow support-based position is commonly used to identify underlying deficiencies in the postural control system (Melzer et al., 2010) and predict the risk of falling (Pajala et al., 2008; Stel et al., 2003). Furthermore, tandem standing is a practical position to assess the ability for uneven weight distribution in individuals with leg-related motor disorders, as more weight is placed on the rear leg (Jonsson et al., 2005). We selected semi-tandem standing for this study to ensure participant’s successful performance.
Thus, the present study aimed to examine the within-day and between-day reliabilities of CoP measures in different standing positions with the influence of motor and cognitive dual-tasking in chronic stroke survivors.
2. Materials and Methods
Study participants
Participants were 16 people with chronic stroke (>6 months post-stroke) who participated in an unpublished clinical trial. Common inclusion criteria were as follows: Ability to stand and walk independently for one minute, ability to hold semi-tandem standing independently for 30 seconds, and no recent limb surgery or uncorrected visual or auditory impairments. The exclusion criteria were as follows: Participants with a score higher than 2 on the modified Ashworth scale in calf muscle (Li et al., 2014), 2), a score lower than 24 on the mini-mental state examination-Persian version (Ansari et al., 2010), a standard deviation (SD) of ±1 or greater on the line bisection test (hemineglect history) (Plummer et al., 2003), and conditions that may affect their balance control except stroke were excluded. Age, height, weight, sex, and type of stroke were obtained from participants. They were also assessed by the Berg balance scale (BBS) (Salavati et al., 2012), the mini-balance evaluation system test (Mini-BEST) (Molhemi et al., 2024), and activities-specific balance confidence (ABC) (Hassan et al., 2015) (Table 1).
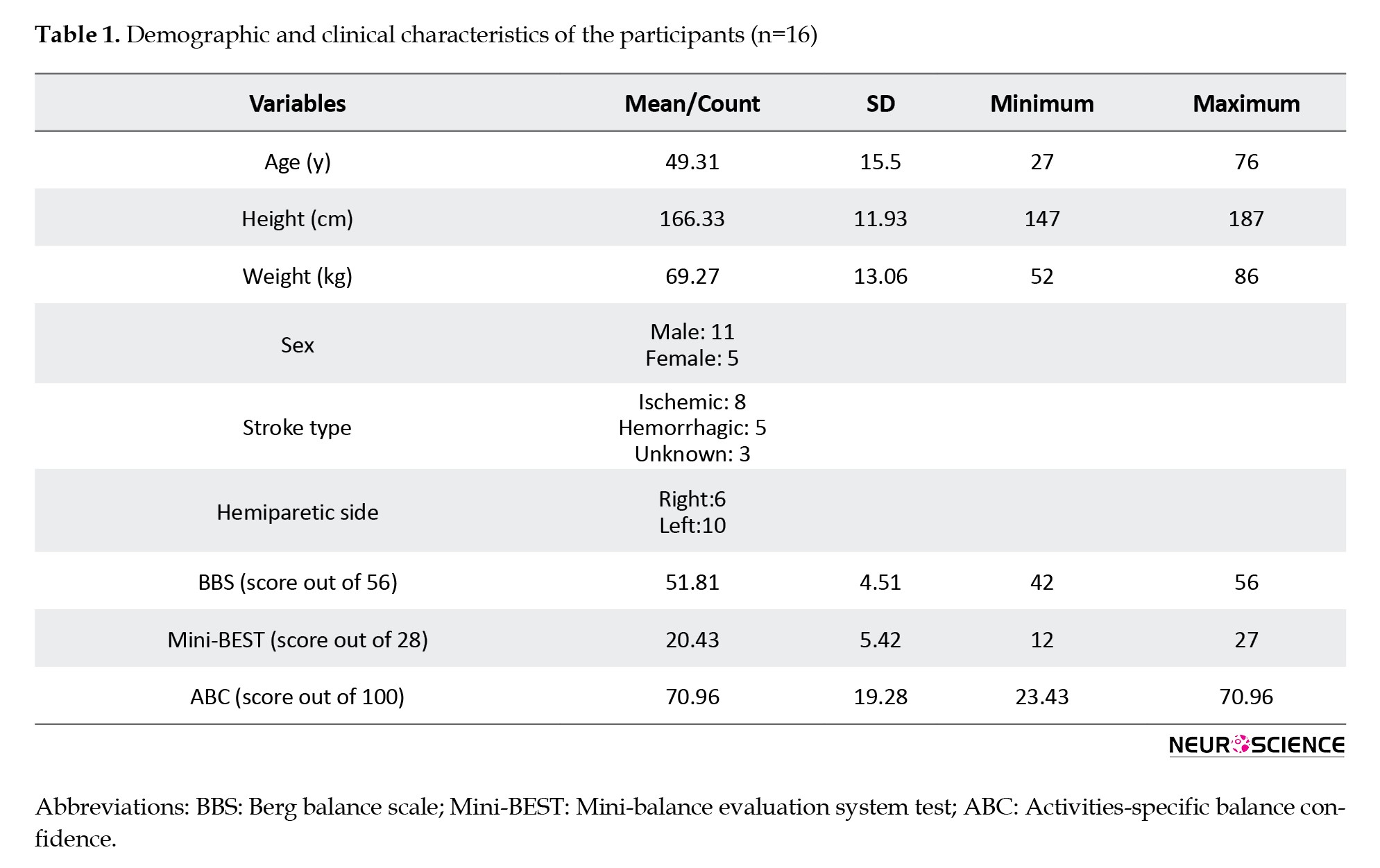
BBS is a valid and reliable 14-item balance assessment tool for stroke patients. Each item is graded on a 5-point scale, and the total score ranges from 0 to 56. The inter-rater reliability (intraclass correlation coefficient [ICC]: 0.98) and the intra-rater reliability (ICC: 0.97) were very high in post-stroke survivors (Berg et al., 1995). Mini-BEST consists of 14 items that assess dynamic balance and have excellent intra-rater reliability (ICC: 0.97) and inter-rater reliability (ICC: 0.96) for stroke patients. Each item is graded on a 3-point scale with a score of 0 to 28 (Tsang et al., 2013). The ABC scale measures the psychological impact of balance impairment and falls. It is a valid and reliable scale (Internal consistency: 0.94 and test re-test reliability ICC: 0.85), rating confidence in performing activities from 0% to 100%. The percentage for each of the 16 items is averaged (Botner et al., 2005).
Study procedure
CoP data were obtained using two adjacent strain gauge Kistler force platforms (model No. 9286BA, Switzerland). Assessments were carried out by the same rater in the exact location and time during two sessions, 48 hours apart, with three trials per session (Gray et al., 2014; Jagroop et al., 2023). The lighting and sound levels of the environment were controlled. Postural sway was measured in three conditions: Single-task, motor dual-task, and cognitive dual-task. In the single-task condition, participants maintained an open-eye quiet standing (open-quiet), an open-eye semi-tandem standing (open-tandem), and a closed-eye quiet standing (closed-quiet). In motor and cognitive dual-task conditions, the participants held quiet and semi-tandem standing (motor-quiet, motor-tandem, and cognitive-quiet, cognitive-tandem, respectively). During quiet standing, they were instructed to stand comfortably barefoot, as still and quiet as possible, on two adjacent force plates with their feet shoulder-width apart, arms at their sides, and gaze at the wall 2 m in front. Both feet were placed on the same plate, with a foot-width distance between them and the affected leg in front, during semi-tandem standing (Jonsson et al., 2005). The position of the feet remained the same throughout all assessment sessions. For motor dual-tasking, participants hold a tray containing a glass of water (Negahban et al., 2017). For cognitive dual-tasking, they conducted the congruent Stroop test, which has been previously validated and proven reliable in its Persian version (Sadri Damirchi et al., 2019). A board with 45 words was placed two meters away from participants for the Stroop task. Words were names of four colors written in the same color ink, and were arranged in 9 rows of 5 words (Negahban et al., 2017). All positions were held for approximately 30 s, with a 30-second break between trials. A physiotherapist supervised participants during assessments for safety.
Data processing
Force platform data were sampled at 100 Hz with a low-pass filter at 10 Hz. A MATLAB routine computed CoP measures for combining both plates (net-CoP). The Mean±SD of net-CoP velocity along anterior-posterior (AP) (Vap and SD.Vap) and medial-lateral (ML) directions (Vml and SD.Vml), mean velocity (Vmean), and sway area (Area) were chosen as their relevance in hemiplegic stroke patients was demonstrated (Gasq et al., 2014), and previously recommended (Palmieri et al., 2002). CoP velocity reflects the efficiency of the postural control system in counteracting postural sway via neuromuscular activity. The SD of velocity is the variability index of CoP velocity (Paillard & Noé, 2015). The lower the velocity and SD, the better the balance control. The sway area quantifies 95% of the ellipse formed by CoP excursion, representing the overall performance of the postural control system. Smaller sway area indicates better balance control performance (Paillard & Noé, 2015).
Statistical analysis
Data analysis was conducted using SPSS software, version 21. A 2-way random model of the (ICC with a corresponding 95% confidence interval (CI) was used to estimate relative reliability. Three assessment trials in a single session were used to examine within-day reliability. The average of 3 trials in 2 separate sessions was implemented for between-day reliability. Munro’s classification for reliability coefficients used to represent the degree of reliability: 0–0.25 – little, if any correlation; 0.26–0.49 – low correlation; 0.5–0.69 – moderate correlation; 0.7–0.89 – high correlation, and 0.9–1 – very high correlation (Munro, 2005). Absolute reliability was determined using the standard error of measurement (SEM). SEM (SD ×indicates how much a change in measurement score is due to random error (Atkinson & Nevill, 1998). The minimal detectable change (MDC) was also calculated (MDC=1.96×√2×SEM), representing a clinically significant change between two measurement scores not due to random error (Atkinson & Nevill, 1998). The statistical significance level was set at 0.05.
3. Results
Demographic characteristics of participants are presented in Table 1.
Table 2 represents the Mean±SD for COP measures under different test conditions.

Within-day reliability
Table 3 presents within-day reliabilities. Generally, within-day ICCs were higher than between-day ICCs.

Single-task condition
ICCs ranged from 0.78 to 0.95, with high to very high reliability for all CoP measures. Lower relative and absolute reliabilities were seen in open-tandem than in open-quiet and closed-quiet positions. Reliabilities of the CoP measures were lower in the closed-quiet than in the open-quiet position, especially in terms of SEMs (0.74-222.39 vs 0.41-96.93, respectively). Sagittal plane measurements (Vap & SD. Vap) had higher reliabilities than the frontal plane (Vml & SD.Vml) in semi-tandem standing (Table 3).
Motor dual-task condition
ICCs ranged from 0.82 to 0.95. All CoP measures had high to very high reliability. Performing a secondary motor task improved the reliabilities of CoP measures in a motor-tandem position (ICC: 0.86-0.95 and SEM: 1.16-1.47) compared to the open-tandem position (ICC: 0.78-0.86 and SEM: 1.42-1.82), except for Area (Table 3).
Cognitive dual-task conditions
ICCs ranged from 0.60 to 0.96. All CoP measures had high to very high reliability, except for the sway area in the cognitive-quiet position. Cognitive dual-tasking improved reliabilities of CoP measures in a cognitive-tandem position (ICC: 0.84-0.98 and SEM: 0.82-1.89) compared to the open-tandem position (ICC: 0.78-0.86 and SEM: 1.33-1.82), except for Area (Table 3).
MDCs ranged from 1.03 mm/s for Vml (cognitive-quiet) to 5.77 mm/s for SD. Vap (closed-quiet), and from 268.60 (open-quiet) to 616.25 (closed-quiet) for Area (Table 3).
Between-day reliability
Table 4 presents between-day reliabilities.

Single-task condition
ICCs ranged from 0.53 to 0.96, with moderate to very high reliability for all CoP measures. The open-tandem position showed lower relative and absolute reliabilities than open-quiet and closed-quiet positions (Table 4). The absolute reliability of CoP measures in a closed-quiet position was almost lower than in an open-quiet position (SEM: 0.99-156.01 versus 0.91-159.17, respectively). Sagittal plane variables had higher reliabilities than the frontal plane variables in open-quiet and open-tandem positions.
Motor dual-task condition
ICCs ranged from 0.83 to 0.94, with high to very high reliability for all CoP measures. Reliabilities were higher in the motor-quiet position than in the motor-tandem position (ICC: 0.90-0.93 and SEM: 0.74-210.61 vs ICC: 0.87-0.92 and SEM: 1.43-245.32, respectively). Again, performing a secondary motor task improved the relative and absolute reliabilities of CoP measures compared to the single-task condition, except for Area (Table 4).
Cognitive dual-task condition
ICCs ranged from 0.66 to 0.96, with high to very high reliability for all CoP measures, except for the Area in the cognitive-quiet position. Cognitive dual-tasking improved the relative and absolute reliabilities of CoP measures compared to the single-task condition, except for Area (Table 4).
MDCs ranged from 1.37 mm/s for Vml (cognitive-quiet) to 7.77 mm/s for SD. Vml (open-tandem) and from 409.06 (cognitive-tandem) to 635.06 (motor-tandem) for Area (Table 4).
4. Discussion
This study aimed to determine the within-day and between-day reliability of COP measures in different standing positions while imposing a motor or cognitive dual-task on the postural control system. Nearly high to very high reliabilities were found for CoP measures. The mean velocity and Mean±SD of velocity in the AP direction showed the highest relative and absolute reliabilities.
Results on mean velocity in the quiet standing mirror before results on healthy elders (Kwon et al., 2022; Moghadam et al., 2011; Ruhe et al., 2010), elderly fallers (Swanenburg et al., 2008), and post-stroke individuals (Gasq et al., 2014; Gray et al., 2014). Mean velocity is more reliable than displacement or sway area, as it is not solely dependent on the CoP position (Gray et al., 2014; Ruhe et al., 2010), and is commonly preferred since it can minimize the extreme effects of peak values (Jagroop et al., 2023). Our findings, especially in dual-task conditions, also confirmed its high reliability.
Additionally, the Mean±SD of velocity in the AP direction were more reliable than in the ML direction in semi-tandem standing. Frontal plane variables are likely less reliable due to stroke survivors’ varying ability to control balance in the ML direction. It is possible that asymmetry in weight bearing, along with difficulty in shifting weight to the affected limb (Gray et al., 2014), resulted in inconsistent measures of CoP in the ML direction across sessions. This inconsistency led to reduced reliability in the variables related to the frontal plane, which is noticeable in the semi-tandem standing position. However, there have been no studies on the reliability of tandem standing in post-stroke individuals. Swanenburg et al. (2008) reported that when stance width increases, a disproportionate decrease occurs in the angular motion of ankles and feet. In semi-tandem standing, the base of support increases in the AP direction, affecting force level variability similar to a broader stance in a side-by-side position (Jonsson et al., 2005). This, in turn, may improve the reliability of sagittal plane variables. Further research could reveal the exact rationale for this finding.
Compared to quiet standing positions, CoP measures in the semi-tandem standing had lower relative and absolute reliability during single-tasking; however, implementing a dual-task assessment enhanced reliability except for the sway area (Tables 3 and 4). It is believed that dual-tasking can improve performance by directing attention toward an external source of attention. This condition leads to automatic motor function, allowing for more effective performance by shifting motor control from higher cognitive to basic noncognitive centers (Ghai et al., 2017). Automating postural control may decrease performance variability and increase the reliability of the measurements. However, further investigations are needed to prove this opinion. Terra et al. (2020) found that reliability decreased in the cognitive dual-task compared to the single-task condition when evaluating patients with Parkinson’s disease. Disagreement is possibly due to significant methodological differences. They studied patients with Parkinson disease, aged 71±7.8 years. They used simple mathematical operations as a secondary task, and participants stood with their back foot’s big toe 5 cm behind the front foot’s heel (Terra et al., 2020). However, based on our study, assessing balance under dual-task conditions provides more reliable CoP measures for diagnosing balance impairments and tracking therapeutic outcomes in chronic post-stroke individuals.
Closing eyes had no significant effect on CoP parameters’ reliability in our study, which aligns with the findings of other studies on post-stroke patients (Gasq et al., 2014) and elders (Li et al., 2016; Lo et al., 2022; Moghadam et al., 2011; Salehi et al., 2010). However, future studies may reveal the exact effect of closing eyes on the reliability of CoP measures when assessing balance in stroke survivors.
Previous research has reported lower reliability for the CoP sway area in stroke patients (Aryan et al., 2023; Gasq et al., 2014; Gray et al., 2014), which contradicts our findings. The lack of research on the sway area of CoP in chronic post-stroke individuals makes it challenging to identify the root of the discrepancy. However, the broad age range of our participants (27 to 76 years) can obscure the test re-test inconsistency; as pointed out by Ruhe et al. (2010), differences in trial duration and foot position may have contributed to inconsistent results. As we found, some studies have shown that sway area is a reliable CoP measure in older adults (18-20, 35, 36) and adults with Parkinson disease (Terra et al., 2020). This outcome could be attributed to some similarities between participants of previous studies and recent populations.
Within-day reliability
Higher within-day ICCs were found than between-day ICCs, consistent with studies on young and old individuals (Benvenuti et al., 1999; Lin et al., 2008; Ruhe et al., 2010). Gray et al. (2014) concluded that averaging ten internal perturbation trials in post-stroke patients improved between-day reliability compared to within-day reliability of CoP measures. However, this population has achieved high within-day reliability in fewer trials (Gray et al., 2014; Jagroop et al., 2023). Fatigue may cause decreased reliability in pathologically affected or elderly individuals during extra trials (Gray et al., 2014; Ruhe et al., 2010).
According to the results, measurements in quiet standing showed high absolute reliability in all three conditions. Jagroop et al. (2023) found lower absolute reliability than our findings in quiet standing in chronic stroke individuals. However, they measured the RMS of CoP velocity. SEM was 4.9 mm for the RMS of Vml and 3.7 mm for the RMS of Vap. Their participants were older (mean age: 64±9.5 years), and they conducted two assessment trials despite identifying that three trials would result in an ICC higher than 0.9 (Jagroop et al., 2023).
In quiet standing, MDCs were lower than in previous results (Aryan et al., 2023). Aryan et al. (2023) investigated the within-session reliability of CoP measures in subacute post-stroke individuals. They reported higher SEMs, and consequently higher MDCs, for Vap and Vml in quiet standing than we found (SEM: 2.83, MDC: 7.84 vs SEM: 0.67, MDC:1.84 for Vap; and SEM: 1.59, MDC:4.41 vs SEM: 0.41, MDC: 1.14 for Vml) (Aryan et al., 2023). It was suggested that balance measures may be less stable among people in early stroke recovery stages (Jagroop et al., 2023), resulting in higher MDCs in their study.
Between-day reliability
Most measures of CoP had high to very high between-day reliability (Table 4). Correspondingly, dual-tasking could increase the reliability of measurements in quiet standing except for the CoP sway area. Gray et al. (2014) found similar results for the load drop task during quiet standing (ICC: 0.78-0.89) than primary quiet standing (ICC: 0.52-0.98). Swanenburg et al. (2008) examined the reliability of CoP measures in fallers and non-fallers under single and dual-task conditions. They reported no significant differences in reliability between test conditions (Swanenburg et al., 2008). However, the mean velocity ICC increased from 0.70 to 0.94 in the fallers performing a secondary cognitive task. Interestingly, they also revealed a decrease in sway area reliability in fallers due to cognitive dual-tasking (ICC 0.69 changed to 0.57), like a study on healthy elders (Moghadam et al., 2011) and our findings. Further investigation is necessary to determine the cause of reduced sway area reliability during dual-task assessment.
It is important to note that the study results may not apply to people other than those with hemiplegic stroke or at different stages of recovery. Additionally, our sample size was limited, which could influence the generalizability of the results, as it may not encompass heterogeneous postural control mechanisms among chronic stroke survivors.
In summary, CoP measures in various positions and conditions are reliable enough to assess balance in chronic stroke survivors. Measuring CoP excursion during dual-task conditions is a more reliable method while evaluating the postural control system, especially in semi-tandem standing. Improving balance assessments by using more reliable measures during dual-tasking can help us understand balance impairments and lead to better rehabilitation interventions.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences, Tehran, Iran (Code: IR.USWR.REC.1398.13664596). All subjects signed an informed consent form before participating in the survey. Participants participated in an unpublished clinical trial (Code: IRCT20220703055350N1).
Funding
This study did not receive funding from any public, commercial, or non-profit organization.
Authors' contributions
Conceptualization and methodology: Mitra Parsa, Mohammad Ali Sanjari, Hossein Negahban, and Iraj Abdollahi; Software: Mohammad Ali Sanjari; Formal analysis: Enayatollah Bakhshi and Mitra Parsa; Investigation: Mitra Parsa and Mohammad Ali Sanjari; Data curation: Haniyeh Fakur Haddadiyan, Mitra Parsa, and Mohammad Ali Sanjari; Resources, and writing the original draft: Mitra Parsa; Review, and editing: Mitra Parsa, Mohammad Ali Sanjari, and Hossein Negahban; Supervision: Mohammad Ali Sanjari, Hossein Negahban, Iraj Abdollahi, and Enayatollah Bakhshi.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank Mohammad Parsa and Payam Sasan Nezhad for contributing to patient selection and the staff of the Rehabilitation Section of the Ghaem Hospital, Mashhad, Iran.
References
Ansari, N. N., Naghdi, S., Hasson, S., Valizadeh, L., & Jalaie, S. (2010). Validation of a Mini-Mental State Examination (MMSE) for the Persian population: A pilot study. Applied Neuropsychology, 17(3), 190–195. [DOI:10.1080/09084282.2010.499773] [PMID]
Arpaia, P., Cuocolo, R., Fullin, A., Gargiulo, L., Mancino, F., & Moccaldi, N., et al. (2024). Executive Functions Assessment Based on Wireless EEG and 3D Gait Analysis During Dual-Task: A Feasibility Study. IEEE Journal of Translational Engineering in Health and Medicine, 12, 268 - 278. [DOI:10.1109/JTEHM.2024.3357287]
Aryan, Inness, E., Patterson, K. K., Mochizuki, G., & Mansfield, A. (2023). Reliability of force plate-based measures of standing balance in the sub-acute stage of post-stroke recovery. Heliyon, 9(10), e21046. [DOI:10.1016/j.heliyon.2023.e21046] [PMID]
Atkinson, G., & Nevill, A. M. (1998). Statistical methods for assessing measurement error (reliability) in variables relevant to sports medicine. Sports Medicine (Auckland, N.Z.), 26(4), 217–238. [DOI:10.2165/00007256-199826040-00002] [PMID]
Benvenuti, F., Mecacci, R., Gineprari, I., Bandinelli, S., Benvenuti, E., & Ferrucci, L., et al. (1999). Kinematic characteristics of standing disequilibrium: Reliability and validity of a posturographic protocol. Archives of Physical Medicine and Rehabilitation, 80(3), 278–287. [DOI:10.1016/S0003-9993(99)90138-7] [PMID]
Berg, K., Wood-Dauphinee, S., & Williams, J. I. (1995). The Balance Scale: Reliability assessment with elderly residents and patients with an acute stroke. Scandinavian Journal of Rehabilitation Medicine, 27(1), 27–36. [DOI:10.2340/1650197719952736] [PMID]
Bernhardt, J., Hayward, K. S., Kwakkel, G., Ward, N. S., Wolf, S. L., & Borschmann, K., et al. (2017). Agreed definitions and a shared vision for new standards in stroke recovery research: The stroke recovery and rehabilitation roundtable taskforce. International Journal of Stroke, 12(5), 444-450. [DOI:10.1177/1747493017711816] [PMID]
Botner, E. M., Miller, W. C., & Eng, J. J. (2005). Measurement properties of the activities-specific balance Confidence Scale among individuals with stroke. Disability and Rehabilitation, 27(4), 156–163. [DOI:10.1080/09638280400008982] [PMID]
Bower, K. J., McGinley, J. L., Miller, K. J., & Clark, R. A. (2014). Instrumented static and dynamic balance assessment after stroke using Wii Balance Boards: Reliability and association with clinical tests. Plos One, 9(12), e115282. [DOI:10.1371/journal.pone.0115282] [PMID]
Corriveau, H., Hébert, R., Raîche, M., & Prince, F. (2004). Evaluation of postural stability in the elderly with stroke. Archives of Physical Medicine and Rehabilitation, 85(7), 1095–1101. [DOI:10.1016/j.apmr.2003.09.023] [PMID]
Fullin, A., Caravaggi, P., Picerno, P., Mosca, M., Caravelli, S., & De Luca, A., et al. (2022). Variability of postural stability and plantar pressure parameters in healthy subjects evaluated by a novel pressure plate. International Journal of Environmental Research and Public Health, 19(5), 2913. [DOI:10.3390/ijerph19052913] [PMID]
Gasq, D., Labrunée, M., Amarantini, D., Dupui, P., Montoya, R., & Marque, P. (2014). Between-day reliability of centre of pressure measures for balance assessment in hemiplegic stroke patients. Journal of Neuroengineering and Rehabilitation, 11, 39. [DOI:10.1186/1743-0003-11-39] [PMID]
Ghai, S., Ghai, I., & Effenberg, A. O. (2017). Effects of dual tasks and dual-task training on postural stability: A systematic review and meta-analysis. Clinical Interventions in Aging, 12, 557–577. [DOI:10.2147/CIA.S125201] [PMID]
Gray, V. L., Ivanova, T. D., & Garland, S. J. (2014). Reliability of center of pressure measures within and between sessions in individuals post-stroke and healthy controls. Gait & Posture, 40(1), 198–203. [DOI:10.1016/j.gaitpost.2014.03.191] [PMID]
Hassan, H., Zarrinkoob, H., Jafarzadeh, S., &Akbarzade Baghban, A. (2015). Psychometric evaluation of Persian version of activities-specific balance confidence scale for elderly Persians. Auditory and Vestibular Research Journal, 24(2), 54-63. [Link]
Jagroop, D., Aryan, R., Schinkel-Ivy, A., & Mansfield, A. (2023). Reliability of unconventional centre of pressure measures of quiet standing balance in people with chronic stroke. Gait & Posture, 102, 159-163. [DOI:10.1016/j.gaitpost.2023.03.021] [PMID]
Jette, D. U., Halbert, J., Iverson, C., Miceli, E., & Shah, P. (2009). Use of standardized outcome measures in physical therapist practice: Perceptions and applications. Physical Therapy, 89(2), 125-135. [DOI:10.2522/ptj.20080234]
Jonsson, E., Seiger, A., & Hirschfeld, H. (2005). Postural steadiness and weight distribution during tandem stance in healthy young and elderly adults. Clinical Biomechanics (Bristol, Avon), 20(2), 202–208. [DOI:10.1016/j.clinbiomech.2004.09.008] [PMID]
Kahya, M., Moon, S., Ranchet, M., Vukas, R. R., Lyons, K. E., & Pahwa, R., et al. (2019). Brain activity during dual task gait and balance in aging and age-related neurodegenerative conditions: A systematic review. Experimental Gerontology, 128, 110756. [DOI:10.1016/j.exger.2019.110756] [PMID]
Kwon, Y. R., Eom, G. M., & Kim, J. W. (2022). Test re-test reliability of postural sway measures during static standing balance performance in healthy elderly adults. Journal of Mechanics in Medicine and Biology, 22(08), 2240034. [DOI:10.1142/S0219519422400346]
Lafond, D., Corriveau, H., Hébert, R., & Prince, F. (2004). Intrasession reliability of center of pressure measures of postural steadiness in healthy elderly people. Archives of Physical Medicine and Rehabilitation, 85(6), 896–901. [DOI:10.1016/j.apmr.2003.08.089] [PMID]
Li, F., Wu, Y., & Li, X. (2014). test re-test reliability and inter-rater reliability of the Modified Tardieu Scale and the Modified Ashworth Scale in hemiplegic patients with stroke. European Journal of Physical and Rehabilitation Medicine, 50(1), 9–15. [PMID]
Li, Z., Liang, Y. Y., Wang, L., Sheng, J., & Ma, S. J. (2016). Reliability and validity of center of pressure measures for balance assessment in older adults. Journal of Physical Therapy Science, 28(4), 1364–1367. [DOI:10.1589/jpts.28.1364] [PMID]
Lin, D., Seol, H., Nussbaum, M. A., & Madigan, M. L. (2008). Reliability of COP-based postural sway measures and age-related differences. Gait & Posture, 28(2), 337–342. [DOI:10.1016/j.gaitpost.2008.01.005] [PMID]
Lo, P. Y., Su, B. L., You, Y. L., Yen, C. W., Wang, S. T., & Guo, L. Y. (2022). Measuring the Reliability of Postural Sway Measurements for a Static Standing Task: The effect of age. Frontiers in Physiology, 13, 850707. [DOI:10.3389/fphys.2022.850707] [PMID]
Mansfield, A., & Inness, E. L. (2015). Force plate assessment of quiet standing balance control: Perspectives on clinical application within stroke rehabilitation. Advances in Rehabilitation Science and Practice, 2015, 4. [DOI:10.4137/RPO.S20363]
Martello, S. K., Boumer, T. C., Almeida, J. C. D., Correa, K. P., Devetak, G. F., & Faucz, R., et al. (2017). Reliability and minimal detectable change of between-limb synchronization, weight-bearing symmetry, and amplitude of postural sway in individuals with stroke. Research on Biomedical Engineering, 33(2), 113-120. [DOI:10.1590/2446-4740.06816]
Melzer, I., Benjuya, N., & Kaplanski, J. (2004). Postural stability in the elderly: A comparison between fallers and non-fallers. Age and Ageing, 33(6), 602–607. [DOI:10.1093/ageing/afh218] [PMID]
Melzer, I., Kurz, I., & Oddsson, L. I. (2010). A retrospective analysis of balance control parameters in elderly fallers and non-fallers. Clinical Biomechanics (Bristol, Avon), 25(10), 984–988.[DOI:10.1016/j.clinbiomech.2010.07.007] [PMID]
Moghadam, M., Ashayeri, H., Salavati, M., Sarafzadeh, J., Taghipoor, K. D., & Saeedi, A., et al. (2011). Reliability of center of pressure measures of postural stability in healthy older adults: Effects of postural task difficulty and cognitive load. Gait & Posture, 33(4), 651–655. [DOI:10.1016/j.gaitpost.2011.02.016] [PMID]
Mohammadi-Rad, S., Mohseni Bandpei, M. A., Salavati, M., Talebian, S., Keyhani, S., & Shanbehzadeh, S. (2022). Reliability of Center of pressure measures of postural stability in anterior cruciate ligament reconstructed athletes: Effect of vibration and cognitive load. The Archives of Bone and Joint Surgery, 10(2), 171–182. [PMID]
Molhemi, F., Monjezi, S., Mehravar, M., Shaterzadeh-Yazdi, M. J., & Majdinasab, N. (2024). Validity, reliability, and responsiveness of Persian version of mini-balance evaluation system test among ambulatory people with multiple sclerosis. Physiotherapy Theory and Practice, 40(3), 565–575. [DOI:10.1080/09593985.2022.2119908] [PMID]
Munro, B. H. (2005). Statistical methods for health care research. Pennsylvania: Lippincott Williams & Wilkins. [Link]
Negahban, H., Ebrahimzadeh, M., & Mehravar, M. (2017). The effects of cognitive versus motor demands on postural performance and weight bearing asymmetry in patients with stroke. Neuroscience Letters, 659, 75–79. [DOI:10.1016/j.neulet.2017.08.070] [PMID]
Paillard, T., & Noé, F. (2015). Techniques and Methods for Testing the Postural Function in Healthy and Pathological Subjects. BioMed Research International, 2015, 891390.[DOI:10.1155/2015/891390] [PMID]
Pajala, S., Era, P., Koskenvuo, M., Kaprio, J., Törmäkangas, T., & Rantanen, T. (2008). Force platform balance measures as predictors of indoor and outdoor falls in community-dwelling women aged 63-76 years. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 63(2), 171–178. [DOI:10.1093/gerona/63.2.171] [PMID]
Palmieri, R. M., Ingersoll, C. D., Stone, M. B., & Krause, B. A. (2002). Center-of-pressure parameters used in the assessment of postural control. Journal of Sport Rehabilitation, 11(1), 51-66. [Link]
Plummer, P., Morris, M. E., & Dunai, J. (2003). Assessment of unilateral neglect. Physical Therapy, 83(8), 732–740. [PMID]
Ruhe, A., Fejer, R., & Walker, B. (2010). The test-retest reliability of centre of pressure measures in bipedal static task conditions--a systematic review of the literature. Gait & Posture, 32(4), 436–445. [DOI:10.1016/j.gaitpost.2010.09.012] [PMID]
Sackley, C. M. (1991). Falls, sway, and symmetry of weight-bearing after stroke. International Disability Studies, 13(1), 1-4. [DOI:10.3109/03790799109166267] [PMID]
Sadri Damirchi, E., Akbari, T., Mojarad, A., & Behbuei, S. (2019). [The role of stroop performance in predicting sleep quality and quality of life in the elderly (Persian)]. Iranian Journal of Ageing, 13(5), 564-575. [DOI:10.32598/SIJA.13.Special-Issue.564]
Salavati, M., Hadian, M. R., Mazaheri, M., Negahban, H., Ebrahimi, I., & Talebian, S., et al. (2009). test re-test reliabty of center of pressure measures of postural stability during quiet standing in a group with musculoskeletal disorders consisting of low back pain, anterior cruciate ligament injury and functional ankle instability. Gait & Posture, 29(3), 460-464. [DOI:10.1016/j.gaitpost.2008.11.016] [PMID]
Salavati, M., Negahban, H., Mazaheri, M., Soleimanifar, M., Hadadi, M., &Sefiddashti, L., et al. (2012). The Persian version of the berg balance scale: Inter and intra-rater reliability and construct validity in elderly adults. Disability and Rehabilitation, 34(20), 1695-1698. [DOI:10.3109/09638288.2012.660604] [PMID]
Salehi, R., Ebrahimi-Takamjani, I., Esteki, A., Maroufi, N., Parnianpour, M. (2010). Test-retest reliability and minimal detectable change for center of pressure measures of postural stability in elderly subjects. Medical Journal of The Islamic Republic of Iran (MJIRI), 23 (4),224-232. [Link]
Sawacha, Z., Carraro, E., Contessa, P., Guiotto, A., Masiero, S., & Cobelli, C. (2013). Relationship between clinical and instrumental balance assessments in chronic post-stroke hemiparesis subjects. Journal of Neuroengineering and Rehabilitation, 10, 95. [DOI:10.1186/1743-0003-10-95] [PMID]
Stel, V. S., Smit, J. H., Pluijm, S. M., & Lips, P. (2003). Balance and mobility performance as treatable risk factors for recurrent falling in older persons. Journal of Clinical Epidemiology, 56(7), 659–668. [DOI:10.1016/S0895-4356(03)00082-9] [PMID]
Swanenburg, J., de Bruin, E. D., Favero, K., Uebelhart, D., & Mulder, T. (2008). The reliability of postural balance measures in single and dual tasking in elderly fallers and non-fallers. BMC Musculoskeletal Disorders, 9, 162. [DOI:10.1186/1471-2474-9-162] [PMID]
Terra, M. B., Da Silva, R. A., Bueno, M. E. B., Ferraz, H. B., & Smaili, S. M. (2020). Center of pressure-based balance evaluation in individuals with Parkinson's disease: A reliability study. Physiotherapy Theory and Practice, 36(7), 826–833. [DOI:10.1080/09593985.2018.1508261] [PMID]
Tisserand, R., Armand, S., Allali, G., Schnider, A., & Baillieul, S. (2018). Cognitive-motor dual-task interference modulates mediolateral dynamic stability during gait in post-stroke individuals. Human Movement Science, 58, 175–184. [DOI:10.1016/j.humov.2018.01.012] [PMID]
Tsang, C. S., Liao, L. R., Chung, R. C., & Pang, M. Y. (2013). Psychometric properties of the mini-balance evaluation systems test (Mini-BESTest) in community-dwelling individuals with chronic stroke. Physical Therapy, 93(8), 1102–1115. [DOI:10.2522/ptj.20120454] [PMID]
Approximately 50% of stroke survivors experience residual physical disabilities (Corriveau et al., 2004; Sawacha et al., 2013), leading to deficits in sensory, musculoskeletal, perceptual, and cognitive systems, affecting balance control and finally increasing the risk of falls (Corriveau et al., 2004; Jagroop et al., 2023; Sawacha et al., 2013). Therefore, the primary goal of stroke rehabilitation is to enhance balance control, requiring reliable balance measures to guide rehabilitation and monitor progress over time (Jette et al, 2009; Mansfield & Inness, 2015). Clinical balance scales fail to reveal underlying dyscontrol, which could potentially increase the risk of falling as the compensatory strategies used to complete tasks remain unknown (Mansfield & Inness, 2015).
The solution could be to record the center of pressure (CoP) excursion using a force platform in a laboratory setting (Jette et al., 2009; Sackley, 1991; Sawacha et al., 2013). CoP parameters can differentiate between fallers and non-fallers (Melzer et al., 2004; Melzeret al., 2010; Pajala et al., 2008) and are associated with clinical outcome measures in elderly and post-stroke individuals (Sawacha et al., 2013), but the intrinsic variability of CoP measures influences their reliability in postural control assessments. Additionally, reliability is not a static characteristic and varies based on the population (Gasq et al., 2014; Lafond et al., 2004).
To date, several studies have demonstrated acceptable CoP measures reliability in assessing balance in populations with disequilibrium problems (Mohammadi-Rad et al., 2022; Ruhe et al., 2010; Salavati et al., 2009; Terra et al., 2020), healthy elders (Lin et al., 2008; Moghadam et al., 2011; Salehi et al., 2010), and young adults (Fullin et al., 2022; Lo et al., 2022). Few studies have reported it throughout various stages of post-stroke recovery (Bower et al., 2014; Gasq et al., 2014; Gray et al., 2014; Martello et al., 2017). It is worth noting that only one study has specifically examined the reliability of CoP-based variables among chronic stroke survivors, in which a limited number of conventional variables were selected as a part of the main objective (Jagroop et al., 2023). However, during the chronic stage of stroke recovery, rehabilitative interventions have a significant net effect on the patient’s improvement, as spontaneous brain recovery has almost plateaued (Bernhardt et al., 2017). Accordingly, assessing the reliability of CoP measures in the chronic stage of stroke recovery could provide deeper insights into clinical decision-making and upcoming research.
Individuals have limited cognitive capacity based on the attentional capacity theory (Kahya et al., 2019), so they cannot perform two simultaneous tasks efficiently, known as the dual-task effect (Arpaia et al., 2024). Research has indicated that older adults and individuals with age-related neurodegenerative conditions experience higher costs of dual-tasking (Kahya et al., 2019). This condition leads to an elevated risk of falls and loss of independence (Arpaia et al., 2024; Kahya et al., 2019), particularly in post-stroke individuals compared to healthy adults (Tisserand et al., 2018). It is notable that dual-tasking also leads to spatiotemporal locomotor adaptations, which may help post-stroke individuals maintain their balance during dual-task conditions (Ghai et al., 2017; Tisserand et al., 2018). Consequently, monitoring the balance control system during dual-tasking could be beneficial for a more accurate impairment diagnosis and tracking of rehabilitation outcomes. So far, a study has examined the reliability of CoP measures during different postural stability tasks in post-stroke patients, regardless of the influence of dual-tasking on CoP measures reliability (Gray et al., 2014). Therefore, in this study, we investigated the reliability of CoP measures under various dual-task conditions.
Moreover, the reliability of CoP measures in tandem standing in post-stroke individuals has not been studied. However, this narrow support-based position is commonly used to identify underlying deficiencies in the postural control system (Melzer et al., 2010) and predict the risk of falling (Pajala et al., 2008; Stel et al., 2003). Furthermore, tandem standing is a practical position to assess the ability for uneven weight distribution in individuals with leg-related motor disorders, as more weight is placed on the rear leg (Jonsson et al., 2005). We selected semi-tandem standing for this study to ensure participant’s successful performance.
Thus, the present study aimed to examine the within-day and between-day reliabilities of CoP measures in different standing positions with the influence of motor and cognitive dual-tasking in chronic stroke survivors.
2. Materials and Methods
Study participants
Participants were 16 people with chronic stroke (>6 months post-stroke) who participated in an unpublished clinical trial. Common inclusion criteria were as follows: Ability to stand and walk independently for one minute, ability to hold semi-tandem standing independently for 30 seconds, and no recent limb surgery or uncorrected visual or auditory impairments. The exclusion criteria were as follows: Participants with a score higher than 2 on the modified Ashworth scale in calf muscle (Li et al., 2014), 2), a score lower than 24 on the mini-mental state examination-Persian version (Ansari et al., 2010), a standard deviation (SD) of ±1 or greater on the line bisection test (hemineglect history) (Plummer et al., 2003), and conditions that may affect their balance control except stroke were excluded. Age, height, weight, sex, and type of stroke were obtained from participants. They were also assessed by the Berg balance scale (BBS) (Salavati et al., 2012), the mini-balance evaluation system test (Mini-BEST) (Molhemi et al., 2024), and activities-specific balance confidence (ABC) (Hassan et al., 2015) (Table 1).
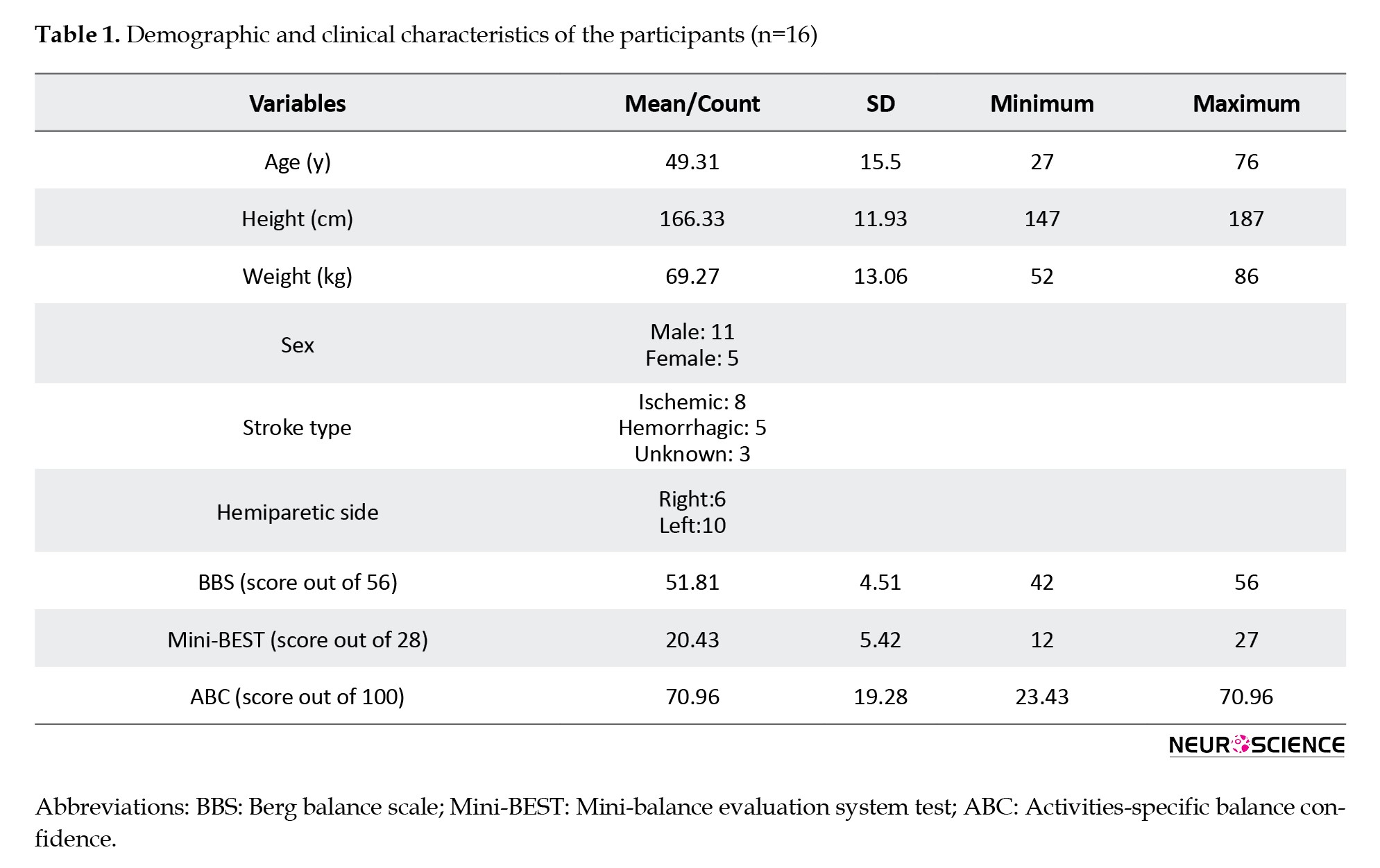
BBS is a valid and reliable 14-item balance assessment tool for stroke patients. Each item is graded on a 5-point scale, and the total score ranges from 0 to 56. The inter-rater reliability (intraclass correlation coefficient [ICC]: 0.98) and the intra-rater reliability (ICC: 0.97) were very high in post-stroke survivors (Berg et al., 1995). Mini-BEST consists of 14 items that assess dynamic balance and have excellent intra-rater reliability (ICC: 0.97) and inter-rater reliability (ICC: 0.96) for stroke patients. Each item is graded on a 3-point scale with a score of 0 to 28 (Tsang et al., 2013). The ABC scale measures the psychological impact of balance impairment and falls. It is a valid and reliable scale (Internal consistency: 0.94 and test re-test reliability ICC: 0.85), rating confidence in performing activities from 0% to 100%. The percentage for each of the 16 items is averaged (Botner et al., 2005).
Study procedure
CoP data were obtained using two adjacent strain gauge Kistler force platforms (model No. 9286BA, Switzerland). Assessments were carried out by the same rater in the exact location and time during two sessions, 48 hours apart, with three trials per session (Gray et al., 2014; Jagroop et al., 2023). The lighting and sound levels of the environment were controlled. Postural sway was measured in three conditions: Single-task, motor dual-task, and cognitive dual-task. In the single-task condition, participants maintained an open-eye quiet standing (open-quiet), an open-eye semi-tandem standing (open-tandem), and a closed-eye quiet standing (closed-quiet). In motor and cognitive dual-task conditions, the participants held quiet and semi-tandem standing (motor-quiet, motor-tandem, and cognitive-quiet, cognitive-tandem, respectively). During quiet standing, they were instructed to stand comfortably barefoot, as still and quiet as possible, on two adjacent force plates with their feet shoulder-width apart, arms at their sides, and gaze at the wall 2 m in front. Both feet were placed on the same plate, with a foot-width distance between them and the affected leg in front, during semi-tandem standing (Jonsson et al., 2005). The position of the feet remained the same throughout all assessment sessions. For motor dual-tasking, participants hold a tray containing a glass of water (Negahban et al., 2017). For cognitive dual-tasking, they conducted the congruent Stroop test, which has been previously validated and proven reliable in its Persian version (Sadri Damirchi et al., 2019). A board with 45 words was placed two meters away from participants for the Stroop task. Words were names of four colors written in the same color ink, and were arranged in 9 rows of 5 words (Negahban et al., 2017). All positions were held for approximately 30 s, with a 30-second break between trials. A physiotherapist supervised participants during assessments for safety.
Data processing
Force platform data were sampled at 100 Hz with a low-pass filter at 10 Hz. A MATLAB routine computed CoP measures for combining both plates (net-CoP). The Mean±SD of net-CoP velocity along anterior-posterior (AP) (Vap and SD.Vap) and medial-lateral (ML) directions (Vml and SD.Vml), mean velocity (Vmean), and sway area (Area) were chosen as their relevance in hemiplegic stroke patients was demonstrated (Gasq et al., 2014), and previously recommended (Palmieri et al., 2002). CoP velocity reflects the efficiency of the postural control system in counteracting postural sway via neuromuscular activity. The SD of velocity is the variability index of CoP velocity (Paillard & Noé, 2015). The lower the velocity and SD, the better the balance control. The sway area quantifies 95% of the ellipse formed by CoP excursion, representing the overall performance of the postural control system. Smaller sway area indicates better balance control performance (Paillard & Noé, 2015).
Statistical analysis
Data analysis was conducted using SPSS software, version 21. A 2-way random model of the (ICC with a corresponding 95% confidence interval (CI) was used to estimate relative reliability. Three assessment trials in a single session were used to examine within-day reliability. The average of 3 trials in 2 separate sessions was implemented for between-day reliability. Munro’s classification for reliability coefficients used to represent the degree of reliability: 0–0.25 – little, if any correlation; 0.26–0.49 – low correlation; 0.5–0.69 – moderate correlation; 0.7–0.89 – high correlation, and 0.9–1 – very high correlation (Munro, 2005). Absolute reliability was determined using the standard error of measurement (SEM). SEM (SD ×indicates how much a change in measurement score is due to random error (Atkinson & Nevill, 1998). The minimal detectable change (MDC) was also calculated (MDC=1.96×√2×SEM), representing a clinically significant change between two measurement scores not due to random error (Atkinson & Nevill, 1998). The statistical significance level was set at 0.05.
3. Results
Demographic characteristics of participants are presented in Table 1.
Table 2 represents the Mean±SD for COP measures under different test conditions.

Within-day reliability
Table 3 presents within-day reliabilities. Generally, within-day ICCs were higher than between-day ICCs.

Single-task condition
ICCs ranged from 0.78 to 0.95, with high to very high reliability for all CoP measures. Lower relative and absolute reliabilities were seen in open-tandem than in open-quiet and closed-quiet positions. Reliabilities of the CoP measures were lower in the closed-quiet than in the open-quiet position, especially in terms of SEMs (0.74-222.39 vs 0.41-96.93, respectively). Sagittal plane measurements (Vap & SD. Vap) had higher reliabilities than the frontal plane (Vml & SD.Vml) in semi-tandem standing (Table 3).
Motor dual-task condition
ICCs ranged from 0.82 to 0.95. All CoP measures had high to very high reliability. Performing a secondary motor task improved the reliabilities of CoP measures in a motor-tandem position (ICC: 0.86-0.95 and SEM: 1.16-1.47) compared to the open-tandem position (ICC: 0.78-0.86 and SEM: 1.42-1.82), except for Area (Table 3).
Cognitive dual-task conditions
ICCs ranged from 0.60 to 0.96. All CoP measures had high to very high reliability, except for the sway area in the cognitive-quiet position. Cognitive dual-tasking improved reliabilities of CoP measures in a cognitive-tandem position (ICC: 0.84-0.98 and SEM: 0.82-1.89) compared to the open-tandem position (ICC: 0.78-0.86 and SEM: 1.33-1.82), except for Area (Table 3).
MDCs ranged from 1.03 mm/s for Vml (cognitive-quiet) to 5.77 mm/s for SD. Vap (closed-quiet), and from 268.60 (open-quiet) to 616.25 (closed-quiet) for Area (Table 3).
Between-day reliability
Table 4 presents between-day reliabilities.

Single-task condition
ICCs ranged from 0.53 to 0.96, with moderate to very high reliability for all CoP measures. The open-tandem position showed lower relative and absolute reliabilities than open-quiet and closed-quiet positions (Table 4). The absolute reliability of CoP measures in a closed-quiet position was almost lower than in an open-quiet position (SEM: 0.99-156.01 versus 0.91-159.17, respectively). Sagittal plane variables had higher reliabilities than the frontal plane variables in open-quiet and open-tandem positions.
Motor dual-task condition
ICCs ranged from 0.83 to 0.94, with high to very high reliability for all CoP measures. Reliabilities were higher in the motor-quiet position than in the motor-tandem position (ICC: 0.90-0.93 and SEM: 0.74-210.61 vs ICC: 0.87-0.92 and SEM: 1.43-245.32, respectively). Again, performing a secondary motor task improved the relative and absolute reliabilities of CoP measures compared to the single-task condition, except for Area (Table 4).
Cognitive dual-task condition
ICCs ranged from 0.66 to 0.96, with high to very high reliability for all CoP measures, except for the Area in the cognitive-quiet position. Cognitive dual-tasking improved the relative and absolute reliabilities of CoP measures compared to the single-task condition, except for Area (Table 4).
MDCs ranged from 1.37 mm/s for Vml (cognitive-quiet) to 7.77 mm/s for SD. Vml (open-tandem) and from 409.06 (cognitive-tandem) to 635.06 (motor-tandem) for Area (Table 4).
4. Discussion
This study aimed to determine the within-day and between-day reliability of COP measures in different standing positions while imposing a motor or cognitive dual-task on the postural control system. Nearly high to very high reliabilities were found for CoP measures. The mean velocity and Mean±SD of velocity in the AP direction showed the highest relative and absolute reliabilities.
Results on mean velocity in the quiet standing mirror before results on healthy elders (Kwon et al., 2022; Moghadam et al., 2011; Ruhe et al., 2010), elderly fallers (Swanenburg et al., 2008), and post-stroke individuals (Gasq et al., 2014; Gray et al., 2014). Mean velocity is more reliable than displacement or sway area, as it is not solely dependent on the CoP position (Gray et al., 2014; Ruhe et al., 2010), and is commonly preferred since it can minimize the extreme effects of peak values (Jagroop et al., 2023). Our findings, especially in dual-task conditions, also confirmed its high reliability.
Additionally, the Mean±SD of velocity in the AP direction were more reliable than in the ML direction in semi-tandem standing. Frontal plane variables are likely less reliable due to stroke survivors’ varying ability to control balance in the ML direction. It is possible that asymmetry in weight bearing, along with difficulty in shifting weight to the affected limb (Gray et al., 2014), resulted in inconsistent measures of CoP in the ML direction across sessions. This inconsistency led to reduced reliability in the variables related to the frontal plane, which is noticeable in the semi-tandem standing position. However, there have been no studies on the reliability of tandem standing in post-stroke individuals. Swanenburg et al. (2008) reported that when stance width increases, a disproportionate decrease occurs in the angular motion of ankles and feet. In semi-tandem standing, the base of support increases in the AP direction, affecting force level variability similar to a broader stance in a side-by-side position (Jonsson et al., 2005). This, in turn, may improve the reliability of sagittal plane variables. Further research could reveal the exact rationale for this finding.
Compared to quiet standing positions, CoP measures in the semi-tandem standing had lower relative and absolute reliability during single-tasking; however, implementing a dual-task assessment enhanced reliability except for the sway area (Tables 3 and 4). It is believed that dual-tasking can improve performance by directing attention toward an external source of attention. This condition leads to automatic motor function, allowing for more effective performance by shifting motor control from higher cognitive to basic noncognitive centers (Ghai et al., 2017). Automating postural control may decrease performance variability and increase the reliability of the measurements. However, further investigations are needed to prove this opinion. Terra et al. (2020) found that reliability decreased in the cognitive dual-task compared to the single-task condition when evaluating patients with Parkinson’s disease. Disagreement is possibly due to significant methodological differences. They studied patients with Parkinson disease, aged 71±7.8 years. They used simple mathematical operations as a secondary task, and participants stood with their back foot’s big toe 5 cm behind the front foot’s heel (Terra et al., 2020). However, based on our study, assessing balance under dual-task conditions provides more reliable CoP measures for diagnosing balance impairments and tracking therapeutic outcomes in chronic post-stroke individuals.
Closing eyes had no significant effect on CoP parameters’ reliability in our study, which aligns with the findings of other studies on post-stroke patients (Gasq et al., 2014) and elders (Li et al., 2016; Lo et al., 2022; Moghadam et al., 2011; Salehi et al., 2010). However, future studies may reveal the exact effect of closing eyes on the reliability of CoP measures when assessing balance in stroke survivors.
Previous research has reported lower reliability for the CoP sway area in stroke patients (Aryan et al., 2023; Gasq et al., 2014; Gray et al., 2014), which contradicts our findings. The lack of research on the sway area of CoP in chronic post-stroke individuals makes it challenging to identify the root of the discrepancy. However, the broad age range of our participants (27 to 76 years) can obscure the test re-test inconsistency; as pointed out by Ruhe et al. (2010), differences in trial duration and foot position may have contributed to inconsistent results. As we found, some studies have shown that sway area is a reliable CoP measure in older adults (18-20, 35, 36) and adults with Parkinson disease (Terra et al., 2020). This outcome could be attributed to some similarities between participants of previous studies and recent populations.
Within-day reliability
Higher within-day ICCs were found than between-day ICCs, consistent with studies on young and old individuals (Benvenuti et al., 1999; Lin et al., 2008; Ruhe et al., 2010). Gray et al. (2014) concluded that averaging ten internal perturbation trials in post-stroke patients improved between-day reliability compared to within-day reliability of CoP measures. However, this population has achieved high within-day reliability in fewer trials (Gray et al., 2014; Jagroop et al., 2023). Fatigue may cause decreased reliability in pathologically affected or elderly individuals during extra trials (Gray et al., 2014; Ruhe et al., 2010).
According to the results, measurements in quiet standing showed high absolute reliability in all three conditions. Jagroop et al. (2023) found lower absolute reliability than our findings in quiet standing in chronic stroke individuals. However, they measured the RMS of CoP velocity. SEM was 4.9 mm for the RMS of Vml and 3.7 mm for the RMS of Vap. Their participants were older (mean age: 64±9.5 years), and they conducted two assessment trials despite identifying that three trials would result in an ICC higher than 0.9 (Jagroop et al., 2023).
In quiet standing, MDCs were lower than in previous results (Aryan et al., 2023). Aryan et al. (2023) investigated the within-session reliability of CoP measures in subacute post-stroke individuals. They reported higher SEMs, and consequently higher MDCs, for Vap and Vml in quiet standing than we found (SEM: 2.83, MDC: 7.84 vs SEM: 0.67, MDC:1.84 for Vap; and SEM: 1.59, MDC:4.41 vs SEM: 0.41, MDC: 1.14 for Vml) (Aryan et al., 2023). It was suggested that balance measures may be less stable among people in early stroke recovery stages (Jagroop et al., 2023), resulting in higher MDCs in their study.
Between-day reliability
Most measures of CoP had high to very high between-day reliability (Table 4). Correspondingly, dual-tasking could increase the reliability of measurements in quiet standing except for the CoP sway area. Gray et al. (2014) found similar results for the load drop task during quiet standing (ICC: 0.78-0.89) than primary quiet standing (ICC: 0.52-0.98). Swanenburg et al. (2008) examined the reliability of CoP measures in fallers and non-fallers under single and dual-task conditions. They reported no significant differences in reliability between test conditions (Swanenburg et al., 2008). However, the mean velocity ICC increased from 0.70 to 0.94 in the fallers performing a secondary cognitive task. Interestingly, they also revealed a decrease in sway area reliability in fallers due to cognitive dual-tasking (ICC 0.69 changed to 0.57), like a study on healthy elders (Moghadam et al., 2011) and our findings. Further investigation is necessary to determine the cause of reduced sway area reliability during dual-task assessment.
It is important to note that the study results may not apply to people other than those with hemiplegic stroke or at different stages of recovery. Additionally, our sample size was limited, which could influence the generalizability of the results, as it may not encompass heterogeneous postural control mechanisms among chronic stroke survivors.
In summary, CoP measures in various positions and conditions are reliable enough to assess balance in chronic stroke survivors. Measuring CoP excursion during dual-task conditions is a more reliable method while evaluating the postural control system, especially in semi-tandem standing. Improving balance assessments by using more reliable measures during dual-tasking can help us understand balance impairments and lead to better rehabilitation interventions.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences, Tehran, Iran (Code: IR.USWR.REC.1398.13664596). All subjects signed an informed consent form before participating in the survey. Participants participated in an unpublished clinical trial (Code: IRCT20220703055350N1).
Funding
This study did not receive funding from any public, commercial, or non-profit organization.
Authors' contributions
Conceptualization and methodology: Mitra Parsa, Mohammad Ali Sanjari, Hossein Negahban, and Iraj Abdollahi; Software: Mohammad Ali Sanjari; Formal analysis: Enayatollah Bakhshi and Mitra Parsa; Investigation: Mitra Parsa and Mohammad Ali Sanjari; Data curation: Haniyeh Fakur Haddadiyan, Mitra Parsa, and Mohammad Ali Sanjari; Resources, and writing the original draft: Mitra Parsa; Review, and editing: Mitra Parsa, Mohammad Ali Sanjari, and Hossein Negahban; Supervision: Mohammad Ali Sanjari, Hossein Negahban, Iraj Abdollahi, and Enayatollah Bakhshi.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank Mohammad Parsa and Payam Sasan Nezhad for contributing to patient selection and the staff of the Rehabilitation Section of the Ghaem Hospital, Mashhad, Iran.
References
Ansari, N. N., Naghdi, S., Hasson, S., Valizadeh, L., & Jalaie, S. (2010). Validation of a Mini-Mental State Examination (MMSE) for the Persian population: A pilot study. Applied Neuropsychology, 17(3), 190–195. [DOI:10.1080/09084282.2010.499773] [PMID]
Arpaia, P., Cuocolo, R., Fullin, A., Gargiulo, L., Mancino, F., & Moccaldi, N., et al. (2024). Executive Functions Assessment Based on Wireless EEG and 3D Gait Analysis During Dual-Task: A Feasibility Study. IEEE Journal of Translational Engineering in Health and Medicine, 12, 268 - 278. [DOI:10.1109/JTEHM.2024.3357287]
Aryan, Inness, E., Patterson, K. K., Mochizuki, G., & Mansfield, A. (2023). Reliability of force plate-based measures of standing balance in the sub-acute stage of post-stroke recovery. Heliyon, 9(10), e21046. [DOI:10.1016/j.heliyon.2023.e21046] [PMID]
Atkinson, G., & Nevill, A. M. (1998). Statistical methods for assessing measurement error (reliability) in variables relevant to sports medicine. Sports Medicine (Auckland, N.Z.), 26(4), 217–238. [DOI:10.2165/00007256-199826040-00002] [PMID]
Benvenuti, F., Mecacci, R., Gineprari, I., Bandinelli, S., Benvenuti, E., & Ferrucci, L., et al. (1999). Kinematic characteristics of standing disequilibrium: Reliability and validity of a posturographic protocol. Archives of Physical Medicine and Rehabilitation, 80(3), 278–287. [DOI:10.1016/S0003-9993(99)90138-7] [PMID]
Berg, K., Wood-Dauphinee, S., & Williams, J. I. (1995). The Balance Scale: Reliability assessment with elderly residents and patients with an acute stroke. Scandinavian Journal of Rehabilitation Medicine, 27(1), 27–36. [DOI:10.2340/1650197719952736] [PMID]
Bernhardt, J., Hayward, K. S., Kwakkel, G., Ward, N. S., Wolf, S. L., & Borschmann, K., et al. (2017). Agreed definitions and a shared vision for new standards in stroke recovery research: The stroke recovery and rehabilitation roundtable taskforce. International Journal of Stroke, 12(5), 444-450. [DOI:10.1177/1747493017711816] [PMID]
Botner, E. M., Miller, W. C., & Eng, J. J. (2005). Measurement properties of the activities-specific balance Confidence Scale among individuals with stroke. Disability and Rehabilitation, 27(4), 156–163. [DOI:10.1080/09638280400008982] [PMID]
Bower, K. J., McGinley, J. L., Miller, K. J., & Clark, R. A. (2014). Instrumented static and dynamic balance assessment after stroke using Wii Balance Boards: Reliability and association with clinical tests. Plos One, 9(12), e115282. [DOI:10.1371/journal.pone.0115282] [PMID]
Corriveau, H., Hébert, R., Raîche, M., & Prince, F. (2004). Evaluation of postural stability in the elderly with stroke. Archives of Physical Medicine and Rehabilitation, 85(7), 1095–1101. [DOI:10.1016/j.apmr.2003.09.023] [PMID]
Fullin, A., Caravaggi, P., Picerno, P., Mosca, M., Caravelli, S., & De Luca, A., et al. (2022). Variability of postural stability and plantar pressure parameters in healthy subjects evaluated by a novel pressure plate. International Journal of Environmental Research and Public Health, 19(5), 2913. [DOI:10.3390/ijerph19052913] [PMID]
Gasq, D., Labrunée, M., Amarantini, D., Dupui, P., Montoya, R., & Marque, P. (2014). Between-day reliability of centre of pressure measures for balance assessment in hemiplegic stroke patients. Journal of Neuroengineering and Rehabilitation, 11, 39. [DOI:10.1186/1743-0003-11-39] [PMID]
Ghai, S., Ghai, I., & Effenberg, A. O. (2017). Effects of dual tasks and dual-task training on postural stability: A systematic review and meta-analysis. Clinical Interventions in Aging, 12, 557–577. [DOI:10.2147/CIA.S125201] [PMID]
Gray, V. L., Ivanova, T. D., & Garland, S. J. (2014). Reliability of center of pressure measures within and between sessions in individuals post-stroke and healthy controls. Gait & Posture, 40(1), 198–203. [DOI:10.1016/j.gaitpost.2014.03.191] [PMID]
Hassan, H., Zarrinkoob, H., Jafarzadeh, S., &Akbarzade Baghban, A. (2015). Psychometric evaluation of Persian version of activities-specific balance confidence scale for elderly Persians. Auditory and Vestibular Research Journal, 24(2), 54-63. [Link]
Jagroop, D., Aryan, R., Schinkel-Ivy, A., & Mansfield, A. (2023). Reliability of unconventional centre of pressure measures of quiet standing balance in people with chronic stroke. Gait & Posture, 102, 159-163. [DOI:10.1016/j.gaitpost.2023.03.021] [PMID]
Jette, D. U., Halbert, J., Iverson, C., Miceli, E., & Shah, P. (2009). Use of standardized outcome measures in physical therapist practice: Perceptions and applications. Physical Therapy, 89(2), 125-135. [DOI:10.2522/ptj.20080234]
Jonsson, E., Seiger, A., & Hirschfeld, H. (2005). Postural steadiness and weight distribution during tandem stance in healthy young and elderly adults. Clinical Biomechanics (Bristol, Avon), 20(2), 202–208. [DOI:10.1016/j.clinbiomech.2004.09.008] [PMID]
Kahya, M., Moon, S., Ranchet, M., Vukas, R. R., Lyons, K. E., & Pahwa, R., et al. (2019). Brain activity during dual task gait and balance in aging and age-related neurodegenerative conditions: A systematic review. Experimental Gerontology, 128, 110756. [DOI:10.1016/j.exger.2019.110756] [PMID]
Kwon, Y. R., Eom, G. M., & Kim, J. W. (2022). Test re-test reliability of postural sway measures during static standing balance performance in healthy elderly adults. Journal of Mechanics in Medicine and Biology, 22(08), 2240034. [DOI:10.1142/S0219519422400346]
Lafond, D., Corriveau, H., Hébert, R., & Prince, F. (2004). Intrasession reliability of center of pressure measures of postural steadiness in healthy elderly people. Archives of Physical Medicine and Rehabilitation, 85(6), 896–901. [DOI:10.1016/j.apmr.2003.08.089] [PMID]
Li, F., Wu, Y., & Li, X. (2014). test re-test reliability and inter-rater reliability of the Modified Tardieu Scale and the Modified Ashworth Scale in hemiplegic patients with stroke. European Journal of Physical and Rehabilitation Medicine, 50(1), 9–15. [PMID]
Li, Z., Liang, Y. Y., Wang, L., Sheng, J., & Ma, S. J. (2016). Reliability and validity of center of pressure measures for balance assessment in older adults. Journal of Physical Therapy Science, 28(4), 1364–1367. [DOI:10.1589/jpts.28.1364] [PMID]
Lin, D., Seol, H., Nussbaum, M. A., & Madigan, M. L. (2008). Reliability of COP-based postural sway measures and age-related differences. Gait & Posture, 28(2), 337–342. [DOI:10.1016/j.gaitpost.2008.01.005] [PMID]
Lo, P. Y., Su, B. L., You, Y. L., Yen, C. W., Wang, S. T., & Guo, L. Y. (2022). Measuring the Reliability of Postural Sway Measurements for a Static Standing Task: The effect of age. Frontiers in Physiology, 13, 850707. [DOI:10.3389/fphys.2022.850707] [PMID]
Mansfield, A., & Inness, E. L. (2015). Force plate assessment of quiet standing balance control: Perspectives on clinical application within stroke rehabilitation. Advances in Rehabilitation Science and Practice, 2015, 4. [DOI:10.4137/RPO.S20363]
Martello, S. K., Boumer, T. C., Almeida, J. C. D., Correa, K. P., Devetak, G. F., & Faucz, R., et al. (2017). Reliability and minimal detectable change of between-limb synchronization, weight-bearing symmetry, and amplitude of postural sway in individuals with stroke. Research on Biomedical Engineering, 33(2), 113-120. [DOI:10.1590/2446-4740.06816]
Melzer, I., Benjuya, N., & Kaplanski, J. (2004). Postural stability in the elderly: A comparison between fallers and non-fallers. Age and Ageing, 33(6), 602–607. [DOI:10.1093/ageing/afh218] [PMID]
Melzer, I., Kurz, I., & Oddsson, L. I. (2010). A retrospective analysis of balance control parameters in elderly fallers and non-fallers. Clinical Biomechanics (Bristol, Avon), 25(10), 984–988.[DOI:10.1016/j.clinbiomech.2010.07.007] [PMID]
Moghadam, M., Ashayeri, H., Salavati, M., Sarafzadeh, J., Taghipoor, K. D., & Saeedi, A., et al. (2011). Reliability of center of pressure measures of postural stability in healthy older adults: Effects of postural task difficulty and cognitive load. Gait & Posture, 33(4), 651–655. [DOI:10.1016/j.gaitpost.2011.02.016] [PMID]
Mohammadi-Rad, S., Mohseni Bandpei, M. A., Salavati, M., Talebian, S., Keyhani, S., & Shanbehzadeh, S. (2022). Reliability of Center of pressure measures of postural stability in anterior cruciate ligament reconstructed athletes: Effect of vibration and cognitive load. The Archives of Bone and Joint Surgery, 10(2), 171–182. [PMID]
Molhemi, F., Monjezi, S., Mehravar, M., Shaterzadeh-Yazdi, M. J., & Majdinasab, N. (2024). Validity, reliability, and responsiveness of Persian version of mini-balance evaluation system test among ambulatory people with multiple sclerosis. Physiotherapy Theory and Practice, 40(3), 565–575. [DOI:10.1080/09593985.2022.2119908] [PMID]
Munro, B. H. (2005). Statistical methods for health care research. Pennsylvania: Lippincott Williams & Wilkins. [Link]
Negahban, H., Ebrahimzadeh, M., & Mehravar, M. (2017). The effects of cognitive versus motor demands on postural performance and weight bearing asymmetry in patients with stroke. Neuroscience Letters, 659, 75–79. [DOI:10.1016/j.neulet.2017.08.070] [PMID]
Paillard, T., & Noé, F. (2015). Techniques and Methods for Testing the Postural Function in Healthy and Pathological Subjects. BioMed Research International, 2015, 891390.[DOI:10.1155/2015/891390] [PMID]
Pajala, S., Era, P., Koskenvuo, M., Kaprio, J., Törmäkangas, T., & Rantanen, T. (2008). Force platform balance measures as predictors of indoor and outdoor falls in community-dwelling women aged 63-76 years. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 63(2), 171–178. [DOI:10.1093/gerona/63.2.171] [PMID]
Palmieri, R. M., Ingersoll, C. D., Stone, M. B., & Krause, B. A. (2002). Center-of-pressure parameters used in the assessment of postural control. Journal of Sport Rehabilitation, 11(1), 51-66. [Link]
Plummer, P., Morris, M. E., & Dunai, J. (2003). Assessment of unilateral neglect. Physical Therapy, 83(8), 732–740. [PMID]
Ruhe, A., Fejer, R., & Walker, B. (2010). The test-retest reliability of centre of pressure measures in bipedal static task conditions--a systematic review of the literature. Gait & Posture, 32(4), 436–445. [DOI:10.1016/j.gaitpost.2010.09.012] [PMID]
Sackley, C. M. (1991). Falls, sway, and symmetry of weight-bearing after stroke. International Disability Studies, 13(1), 1-4. [DOI:10.3109/03790799109166267] [PMID]
Sadri Damirchi, E., Akbari, T., Mojarad, A., & Behbuei, S. (2019). [The role of stroop performance in predicting sleep quality and quality of life in the elderly (Persian)]. Iranian Journal of Ageing, 13(5), 564-575. [DOI:10.32598/SIJA.13.Special-Issue.564]
Salavati, M., Hadian, M. R., Mazaheri, M., Negahban, H., Ebrahimi, I., & Talebian, S., et al. (2009). test re-test reliabty of center of pressure measures of postural stability during quiet standing in a group with musculoskeletal disorders consisting of low back pain, anterior cruciate ligament injury and functional ankle instability. Gait & Posture, 29(3), 460-464. [DOI:10.1016/j.gaitpost.2008.11.016] [PMID]
Salavati, M., Negahban, H., Mazaheri, M., Soleimanifar, M., Hadadi, M., &Sefiddashti, L., et al. (2012). The Persian version of the berg balance scale: Inter and intra-rater reliability and construct validity in elderly adults. Disability and Rehabilitation, 34(20), 1695-1698. [DOI:10.3109/09638288.2012.660604] [PMID]
Salehi, R., Ebrahimi-Takamjani, I., Esteki, A., Maroufi, N., Parnianpour, M. (2010). Test-retest reliability and minimal detectable change for center of pressure measures of postural stability in elderly subjects. Medical Journal of The Islamic Republic of Iran (MJIRI), 23 (4),224-232. [Link]
Sawacha, Z., Carraro, E., Contessa, P., Guiotto, A., Masiero, S., & Cobelli, C. (2013). Relationship between clinical and instrumental balance assessments in chronic post-stroke hemiparesis subjects. Journal of Neuroengineering and Rehabilitation, 10, 95. [DOI:10.1186/1743-0003-10-95] [PMID]
Stel, V. S., Smit, J. H., Pluijm, S. M., & Lips, P. (2003). Balance and mobility performance as treatable risk factors for recurrent falling in older persons. Journal of Clinical Epidemiology, 56(7), 659–668. [DOI:10.1016/S0895-4356(03)00082-9] [PMID]
Swanenburg, J., de Bruin, E. D., Favero, K., Uebelhart, D., & Mulder, T. (2008). The reliability of postural balance measures in single and dual tasking in elderly fallers and non-fallers. BMC Musculoskeletal Disorders, 9, 162. [DOI:10.1186/1471-2474-9-162] [PMID]
Terra, M. B., Da Silva, R. A., Bueno, M. E. B., Ferraz, H. B., & Smaili, S. M. (2020). Center of pressure-based balance evaluation in individuals with Parkinson's disease: A reliability study. Physiotherapy Theory and Practice, 36(7), 826–833. [DOI:10.1080/09593985.2018.1508261] [PMID]
Tisserand, R., Armand, S., Allali, G., Schnider, A., & Baillieul, S. (2018). Cognitive-motor dual-task interference modulates mediolateral dynamic stability during gait in post-stroke individuals. Human Movement Science, 58, 175–184. [DOI:10.1016/j.humov.2018.01.012] [PMID]
Tsang, C. S., Liao, L. R., Chung, R. C., & Pang, M. Y. (2013). Psychometric properties of the mini-balance evaluation systems test (Mini-BESTest) in community-dwelling individuals with chronic stroke. Physical Therapy, 93(8), 1102–1115. [DOI:10.2522/ptj.20120454] [PMID]
Type of Study: Original |
Subject:
Clinical Neuroscience
Received: 2024/09/20 | Accepted: 2024/11/30 | Published: 2025/07/1
Received: 2024/09/20 | Accepted: 2024/11/30 | Published: 2025/07/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |





