Volume 16, Issue 1 (January & February 2025)
BCN 2025, 16(1): 131-142 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Shojaeddin A, Jafarian Namini F, Razzaghi Z, Abbass A, Ghorbani N. Efficacy of Intensive Short-term Dynamic Psychotherapy, Laser Acupuncture, and the Combination in Major Depression. BCN 2025; 16 (1) :131-142
URL: http://bcn.iums.ac.ir/article-1-2827-en.html
URL: http://bcn.iums.ac.ir/article-1-2827-en.html
1- Laser Application in Medical Science Research Center, Shahid Beheshti University of Medical Science, Tehran, Iran.
2- Department of Psychology, Faculty of Psychology and Education, University of Tehran, Tehran, Iran.
3- Department of Psychiatry, Centre for Emotion and Health, Dalhousie University, Halifax, Canada.
2- Department of Psychology, Faculty of Psychology and Education, University of Tehran, Tehran, Iran.
3- Department of Psychiatry, Centre for Emotion and Health, Dalhousie University, Halifax, Canada.
Keywords: Laser acupuncture (LA), Intensive short-term dynamic psychotherapy (ISTDP), Depression, Iran
Full-Text [PDF 674 kb]
| Abstract (HTML)
Full-Text:
1. Introduction
Depression is one of the main causes of the mental disorder burden, which is estimated to affect 300 million people globally (Lépine & Briley, 2011). Depression and other mental health disorders are increasing worldwide (Armbrecht et al., 2020). A World Health Assembly resolution, which was adopted in May 2013, demanded an all-inclusive, coordinated response to mental disorders at a national level. In addition to causing personal human suffering, depression is associated with early mortality from suicide and other diseases (Ay-Woan et al., 2006; Hussenoeder et al., 2021; Khalkhali et al., 2018; Orsolini et al., 2020). In Iran, the 12-month prevalence of major depressive disorder is approximately 12.7% (Fava & Kendler, 2000).
To treat depression, pharmacological and non-pharmacological interventions are used together to increase the effectiveness of interventions and reduce the likelihood of recurrence of the symptoms (Kupfer et al., 2012). However, some side effects of medical interventions such as medication and electroconvulsive therapy reduce a person’s willingness to use or to continue the course of treatment (Husain et al., 2004). On the other hand, in some cases, even after completing the course of treatment, patients do not respond to treatment and continue to suffer from depression (Kubitz et al., 2013). Therefore, finding effective alternative, complementary medical and psychological therapies is necessary.
Complementary and alternative medicine, either as an adjunct to or as a replacement for conventional therapies, is employed in treating people with depression (Van Der Watt et al., 2008). However, their mechanism of action and effectiveness need to be empirically investigated. Acupuncture is a treatment derived from traditional Chinese medicine and has long been used to treat mood disorders, making it a candidate alternative to standard antidepressant medication (Pilkington, 2010). Acupuncture is presumed to work by the unblocking of energies. A systematic review of 29 studies, including 2268 participants, showed that the severity of depression was reduced significantly with the use of acupuncture, and a significant correlation was observed between the number of acupuncture treatments and reduction in the severity of depression (Armour et al., 2019).
The so-called laser acupuncture (LA), using laser light instead of needles to stimulate acupoints, has been promoted for almost three decades. Acupuncturists use needles, but laser therapists use a more non-invasive LA method (Smith et al., 2018). LA has shown clinically and statistically significant effects in reducing depressive symptoms and patients’ emotional distress (Quah-Smith et al., 2013; Taguchi et al., 2019). The effectiveness of LA has been proved in various medical conditions (Quah-Smith et al., 2013; Quah-Smith et al., 2005; Taguchi et al., 2019), but little research, if any, has evaluated its effect on depression with diverse measures for depressive symptoms.
Intensive short-term dynamic psychotherapy (ISTDP) is a form of psychotherapy that originated from psychoanalytic tenets. ISTDP helps patients process blocked emotions that generate anxiety and self-defeating mental/behavioral reactions (defenses). Blocked emotions manifest as unique forms of somatic experiences with energy release when unblocked and processed during therapy (Abbass, 2015). Some studies have shown the efficacy of ISTDP in treating major depression (Abbass, 2006; Caldiroli et al., 2020; Town et al., 2017; Town et al., 2020).
The possibility of increasing ISTDP effectiveness in combination with other treatment modalities like LA is an open question addressed in this study. Such a combination is interesting from the theoretical assumptions of ISTDP and LA. Both therapies work on blocked energies using different rationales and theoretical backgrounds. The two radically different methods of treatment may assume the necessity of unblocking energies to heal depression. Both treatments may assume that the cause of such a disorder as depression is the blockage. ISTDP assumes the blockage of painful mixed feelings due to attachment trauma, especially from childhood, is the cause of mental disorders like depression, while LA assumes the blockage of life energies is the cause of disorders due to constitution and or other factors like nutrition, lifestyle, environment, and so on.
ISTDP and LA may operate synergistically to increase the effectiveness of each treatment. A study, for example, evidenced the effectiveness of ISTDP and LA in treating depression in a limited sample. ISTDP develops a form of higher-order, integrative self-knowledge (Ghorbani et al., 2008). It facilitates the experience of blocked emotions that can cause depressive symptoms while it develops a significant understanding of the relationship between blocked emotions and their related defensive reactions that lead to symptoms. ISTDP, in this way, is a form of shuttling back and forth between experiential and reflective self-knowledge (Ghorbani et al., 2003). Block emotions are energies; when they are free, they can help patients reduce depressive symptoms. On the other hand, LA also works on unblocking energy pathways without symbolizing them as meaningful psychological experiences.
Due to limited research on the use of LA in treating depression and using different complementary treatments along with this modality with unknown effectiveness, more clinical trials with robust methodologies could open a new horizon in treating depression. The questions this current study addresses are 1) Whether LA can help treat depression, 2) Whether it can increase the effectiveness of ISTDP in treating depression, and 3) Whether it can be a suitable substitute for psychotropic medication for depression.
2. Materials and Methods
Study design
This trial used a single-blind, randomized, parallel-group design to examine the efficacy of ISTDP compared with LA and the combination of the two treatments in depressed patients who were not receiving medication or psychological treatment within the prior three months.
Outcome measures
The primary measure of effectiveness was the reduction of depressive symptoms measured by the Persian versions of the Hamilton rating depression scale (HDRS) (Ahmadpanah et al., 2016), Persian structured clinical interview for DSM disorder (SCID-II) (Vandad et al., 2004), and Persian symptom checklist-90 (SCL-90) (Akhavan Abiri & Shairi, 2020; Ardakani et al., 2016).
The HDRS and SCID-II were rated by a clinician blinded to the allocation. SCL-90 was rated by the unblinded patients.
Participant eligibility and recruitment
Volunteer participants were recruited from the “Insight-New” Psychological Center in Tehran City, Iran. The inclusion criteria were as follows: the participants had depressive symptoms with a Persian version of the Beck depression inventory (Dadfar & Kalibatseva, 2016; Ghassemzadeh et al., 2005). With a score of 12 to 30, they consented to attend a three-month follow-up after completing interventions and could provide informed consent. They were not included in the trial if they were suffering from chronic dysthymia, that is, chronic depression of over two years’ duration, hypomania, psychosis, or substance abuse. Furthermore, they were excluded from the study if they had been receiving any psychological treatment or psychotropic medications such as prescribed drugs or herbal supplements in the previous three months. A history of neurological disorders, endocrine disorders, pregnancy, and active suicidal ideation constituted other exclusion criteria. To assess their eligibility, a research assistant who was blind to research allocation subsequently conducted a SCID-II interview with participants. They were excluded if they had any history of psychotic, substance or alcohol abuse, mental retardation and obsessive‐compulsive personality disorder, hypothyroidism, and glandular problems.
Randomization and allocation
We performed a randomized controlled trial on 45 patients with three equal arms (15 patients in each group): Group I) LA, group II) ISTDP, and group III) LA together with ISTDP. Randomization was performed using a block method to generate a random list of allocations in blocks of 6. Enrolled patients were randomly assigned by another research assistant, who was uninvolved in the process of eligibility and recruitment, to one of the three groups, according to the randomized list.
Intervention protocol
LA
Over 8 weeks, 12 interventions were administered by the first author. The first four weeks each consisted of two intervention sessions, and the next four weeks each consisted of one intervention session. The intervention comprised the stimulation of corporal points (LI4, LI11, ST36, ST40, BL18, BL20, BL21, SP4, SP6, LIV3, LIV8, LIV14, GB15, GB20, GB34, REN12, REN17, PC6, DU20, and HT7) and of auricular points (heart, stomach, spleen, shenmen, anti-depression, valium, and master omega) determined according to TCM diagnostics, using continuous contact gallium-aluminum-arsenide (GaAlAs) LA, with an average output power of 200 mw, a wavelength of 980 nm, and a dose of 4 J/point for body acupuncture points and 1J/point for ear acupuncture points.
ISTDP
Over 8 weeks, 12 treatment sessions were administered by the second author. The first four weeks each consisted of two intervention sessions, and the next four weeks each consisted of one intervention session. The intervention comprised one hour of ISTDP, focusing on building anxiety tolerance through specific procedures, including a graded format, deactivating various defense mechanisms, and experiencing underlying mixed feelings in the frameworks of the triangle of conflict and the triangle of person (Abbass, 2015). ISTDP in depression operates by overcoming the shut-down of complex feelings and turning inward to guilt-laden rage. The use of pressure (persistent and focused invitation) to experience complex feelings while monitoring the signaling of the anxiety channels and identification and clarification of self-defeating defenses are the key techniques that ISTDP uses to treat depression (Town et al., 2022).
Combined ISTDP and LA
This group received both interventions daily: LA therapy and ISTDP. The patients of all groups were evaluated six times by the HDRS, SCID-II, and SCL-90: The pre-test, eighth session,12th session, first follow-up (after one month), second follow-up (after two months), and third follow-up (after three months).
Treatment adherence
The treatment of ISTDP was supervised by the final author and was based on the treatment guide reaching through resistance (Abbass, 2015). During the project, the second author, who provided ISTDP, had regular weekly case supervision sessions. The ISTDP therapist had finished core training for ISTDP before the project, with the training of the final author. The treatment of LA was not supervised since the first author was a supervisor of LA in Iran.
Statistical analysis
Data were analyzed using SPSS software, version 26, and scores of all questionnaires were described with Mean±SD. Normality was checked with the Shapiro-Wilks test. The within-subject evaluation was performed using a paired sample t-test and a Wilcoxon test. The three groups were compared using ANOVA (analysis of variance) and the Kruskal-Wallis test. P<0.05 were considered significant. No adverse events happened during the treatments.
3. Results
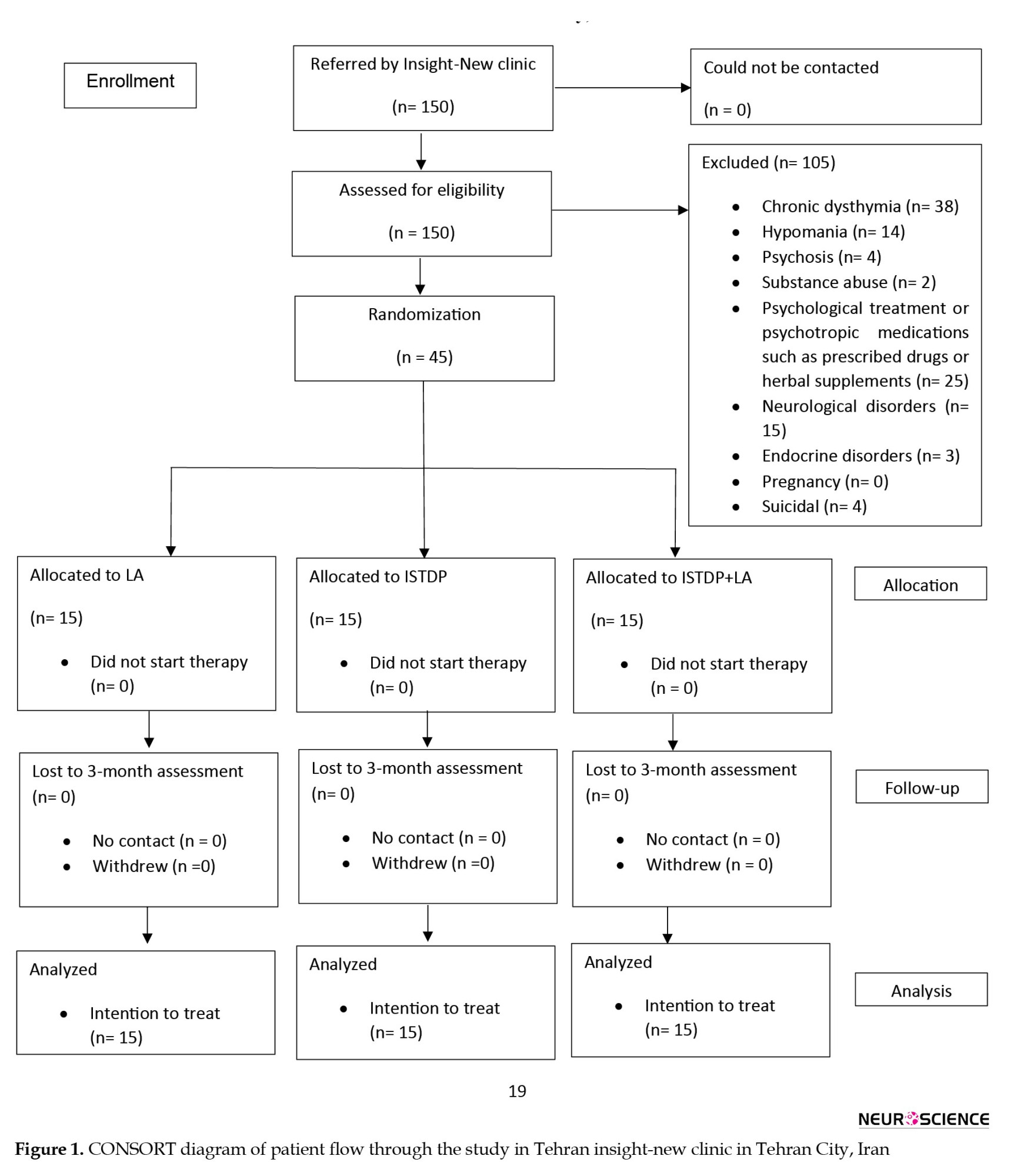
Of nearly 150 patients at the clinic, 45 were included and randomized (Figure 1).
Depression is one of the main causes of the mental disorder burden, which is estimated to affect 300 million people globally (Lépine & Briley, 2011). Depression and other mental health disorders are increasing worldwide (Armbrecht et al., 2020). A World Health Assembly resolution, which was adopted in May 2013, demanded an all-inclusive, coordinated response to mental disorders at a national level. In addition to causing personal human suffering, depression is associated with early mortality from suicide and other diseases (Ay-Woan et al., 2006; Hussenoeder et al., 2021; Khalkhali et al., 2018; Orsolini et al., 2020). In Iran, the 12-month prevalence of major depressive disorder is approximately 12.7% (Fava & Kendler, 2000).
To treat depression, pharmacological and non-pharmacological interventions are used together to increase the effectiveness of interventions and reduce the likelihood of recurrence of the symptoms (Kupfer et al., 2012). However, some side effects of medical interventions such as medication and electroconvulsive therapy reduce a person’s willingness to use or to continue the course of treatment (Husain et al., 2004). On the other hand, in some cases, even after completing the course of treatment, patients do not respond to treatment and continue to suffer from depression (Kubitz et al., 2013). Therefore, finding effective alternative, complementary medical and psychological therapies is necessary.
Complementary and alternative medicine, either as an adjunct to or as a replacement for conventional therapies, is employed in treating people with depression (Van Der Watt et al., 2008). However, their mechanism of action and effectiveness need to be empirically investigated. Acupuncture is a treatment derived from traditional Chinese medicine and has long been used to treat mood disorders, making it a candidate alternative to standard antidepressant medication (Pilkington, 2010). Acupuncture is presumed to work by the unblocking of energies. A systematic review of 29 studies, including 2268 participants, showed that the severity of depression was reduced significantly with the use of acupuncture, and a significant correlation was observed between the number of acupuncture treatments and reduction in the severity of depression (Armour et al., 2019).
The so-called laser acupuncture (LA), using laser light instead of needles to stimulate acupoints, has been promoted for almost three decades. Acupuncturists use needles, but laser therapists use a more non-invasive LA method (Smith et al., 2018). LA has shown clinically and statistically significant effects in reducing depressive symptoms and patients’ emotional distress (Quah-Smith et al., 2013; Taguchi et al., 2019). The effectiveness of LA has been proved in various medical conditions (Quah-Smith et al., 2013; Quah-Smith et al., 2005; Taguchi et al., 2019), but little research, if any, has evaluated its effect on depression with diverse measures for depressive symptoms.
Intensive short-term dynamic psychotherapy (ISTDP) is a form of psychotherapy that originated from psychoanalytic tenets. ISTDP helps patients process blocked emotions that generate anxiety and self-defeating mental/behavioral reactions (defenses). Blocked emotions manifest as unique forms of somatic experiences with energy release when unblocked and processed during therapy (Abbass, 2015). Some studies have shown the efficacy of ISTDP in treating major depression (Abbass, 2006; Caldiroli et al., 2020; Town et al., 2017; Town et al., 2020).
The possibility of increasing ISTDP effectiveness in combination with other treatment modalities like LA is an open question addressed in this study. Such a combination is interesting from the theoretical assumptions of ISTDP and LA. Both therapies work on blocked energies using different rationales and theoretical backgrounds. The two radically different methods of treatment may assume the necessity of unblocking energies to heal depression. Both treatments may assume that the cause of such a disorder as depression is the blockage. ISTDP assumes the blockage of painful mixed feelings due to attachment trauma, especially from childhood, is the cause of mental disorders like depression, while LA assumes the blockage of life energies is the cause of disorders due to constitution and or other factors like nutrition, lifestyle, environment, and so on.
ISTDP and LA may operate synergistically to increase the effectiveness of each treatment. A study, for example, evidenced the effectiveness of ISTDP and LA in treating depression in a limited sample. ISTDP develops a form of higher-order, integrative self-knowledge (Ghorbani et al., 2008). It facilitates the experience of blocked emotions that can cause depressive symptoms while it develops a significant understanding of the relationship between blocked emotions and their related defensive reactions that lead to symptoms. ISTDP, in this way, is a form of shuttling back and forth between experiential and reflective self-knowledge (Ghorbani et al., 2003). Block emotions are energies; when they are free, they can help patients reduce depressive symptoms. On the other hand, LA also works on unblocking energy pathways without symbolizing them as meaningful psychological experiences.
Due to limited research on the use of LA in treating depression and using different complementary treatments along with this modality with unknown effectiveness, more clinical trials with robust methodologies could open a new horizon in treating depression. The questions this current study addresses are 1) Whether LA can help treat depression, 2) Whether it can increase the effectiveness of ISTDP in treating depression, and 3) Whether it can be a suitable substitute for psychotropic medication for depression.
2. Materials and Methods
Study design
This trial used a single-blind, randomized, parallel-group design to examine the efficacy of ISTDP compared with LA and the combination of the two treatments in depressed patients who were not receiving medication or psychological treatment within the prior three months.
Outcome measures
The primary measure of effectiveness was the reduction of depressive symptoms measured by the Persian versions of the Hamilton rating depression scale (HDRS) (Ahmadpanah et al., 2016), Persian structured clinical interview for DSM disorder (SCID-II) (Vandad et al., 2004), and Persian symptom checklist-90 (SCL-90) (Akhavan Abiri & Shairi, 2020; Ardakani et al., 2016).
The HDRS and SCID-II were rated by a clinician blinded to the allocation. SCL-90 was rated by the unblinded patients.
Participant eligibility and recruitment
Volunteer participants were recruited from the “Insight-New” Psychological Center in Tehran City, Iran. The inclusion criteria were as follows: the participants had depressive symptoms with a Persian version of the Beck depression inventory (Dadfar & Kalibatseva, 2016; Ghassemzadeh et al., 2005). With a score of 12 to 30, they consented to attend a three-month follow-up after completing interventions and could provide informed consent. They were not included in the trial if they were suffering from chronic dysthymia, that is, chronic depression of over two years’ duration, hypomania, psychosis, or substance abuse. Furthermore, they were excluded from the study if they had been receiving any psychological treatment or psychotropic medications such as prescribed drugs or herbal supplements in the previous three months. A history of neurological disorders, endocrine disorders, pregnancy, and active suicidal ideation constituted other exclusion criteria. To assess their eligibility, a research assistant who was blind to research allocation subsequently conducted a SCID-II interview with participants. They were excluded if they had any history of psychotic, substance or alcohol abuse, mental retardation and obsessive‐compulsive personality disorder, hypothyroidism, and glandular problems.
Randomization and allocation
We performed a randomized controlled trial on 45 patients with three equal arms (15 patients in each group): Group I) LA, group II) ISTDP, and group III) LA together with ISTDP. Randomization was performed using a block method to generate a random list of allocations in blocks of 6. Enrolled patients were randomly assigned by another research assistant, who was uninvolved in the process of eligibility and recruitment, to one of the three groups, according to the randomized list.
Intervention protocol
LA
Over 8 weeks, 12 interventions were administered by the first author. The first four weeks each consisted of two intervention sessions, and the next four weeks each consisted of one intervention session. The intervention comprised the stimulation of corporal points (LI4, LI11, ST36, ST40, BL18, BL20, BL21, SP4, SP6, LIV3, LIV8, LIV14, GB15, GB20, GB34, REN12, REN17, PC6, DU20, and HT7) and of auricular points (heart, stomach, spleen, shenmen, anti-depression, valium, and master omega) determined according to TCM diagnostics, using continuous contact gallium-aluminum-arsenide (GaAlAs) LA, with an average output power of 200 mw, a wavelength of 980 nm, and a dose of 4 J/point for body acupuncture points and 1J/point for ear acupuncture points.
ISTDP
Over 8 weeks, 12 treatment sessions were administered by the second author. The first four weeks each consisted of two intervention sessions, and the next four weeks each consisted of one intervention session. The intervention comprised one hour of ISTDP, focusing on building anxiety tolerance through specific procedures, including a graded format, deactivating various defense mechanisms, and experiencing underlying mixed feelings in the frameworks of the triangle of conflict and the triangle of person (Abbass, 2015). ISTDP in depression operates by overcoming the shut-down of complex feelings and turning inward to guilt-laden rage. The use of pressure (persistent and focused invitation) to experience complex feelings while monitoring the signaling of the anxiety channels and identification and clarification of self-defeating defenses are the key techniques that ISTDP uses to treat depression (Town et al., 2022).
Combined ISTDP and LA
This group received both interventions daily: LA therapy and ISTDP. The patients of all groups were evaluated six times by the HDRS, SCID-II, and SCL-90: The pre-test, eighth session,12th session, first follow-up (after one month), second follow-up (after two months), and third follow-up (after three months).
Treatment adherence
The treatment of ISTDP was supervised by the final author and was based on the treatment guide reaching through resistance (Abbass, 2015). During the project, the second author, who provided ISTDP, had regular weekly case supervision sessions. The ISTDP therapist had finished core training for ISTDP before the project, with the training of the final author. The treatment of LA was not supervised since the first author was a supervisor of LA in Iran.
Statistical analysis
Data were analyzed using SPSS software, version 26, and scores of all questionnaires were described with Mean±SD. Normality was checked with the Shapiro-Wilks test. The within-subject evaluation was performed using a paired sample t-test and a Wilcoxon test. The three groups were compared using ANOVA (analysis of variance) and the Kruskal-Wallis test. P<0.05 were considered significant. No adverse events happened during the treatments.
3. Results
Of nearly 150 patients at the clinic, 45 were included and randomized (Figure 1).
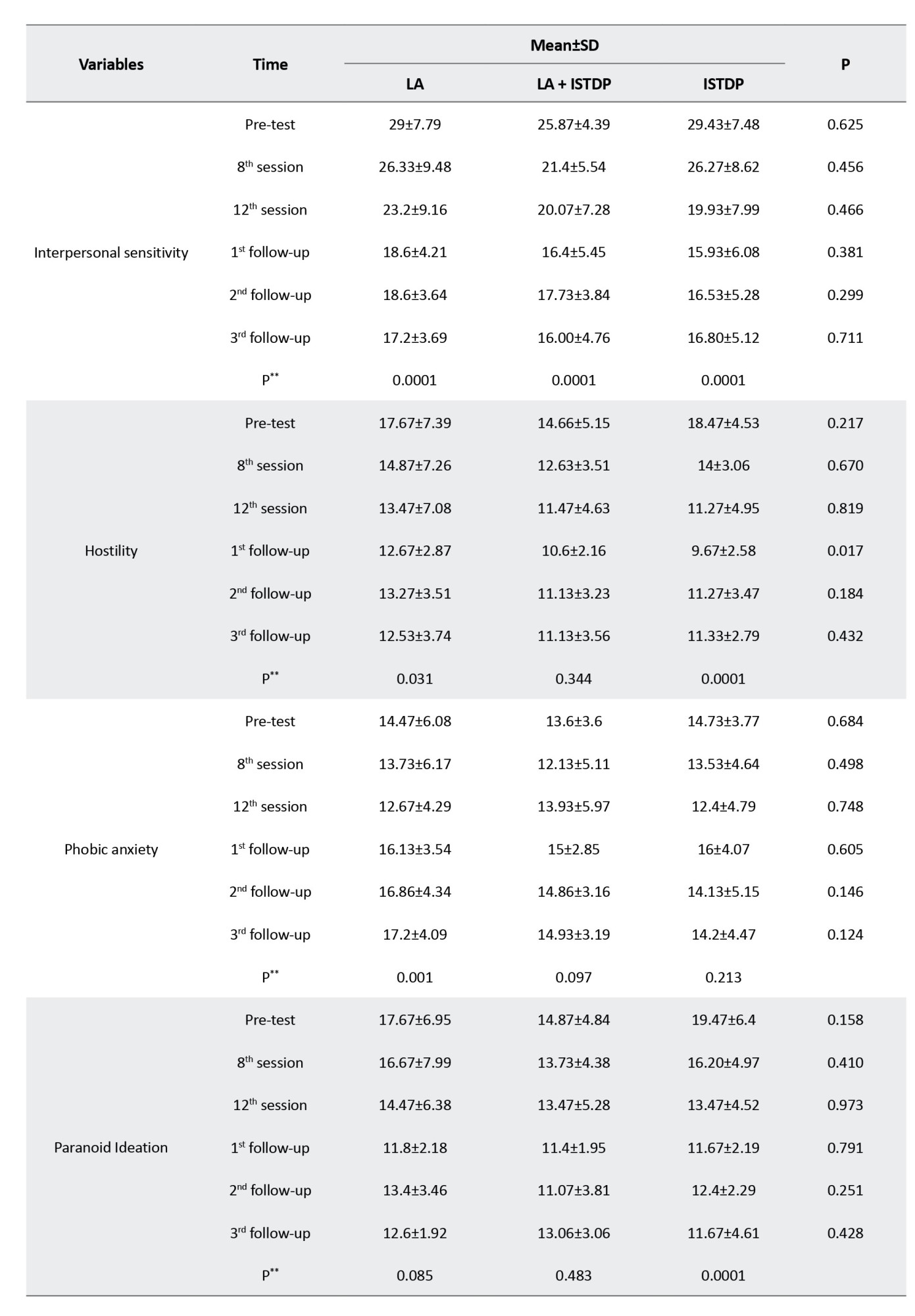
Demographic information for the three groups is described in Table 1.
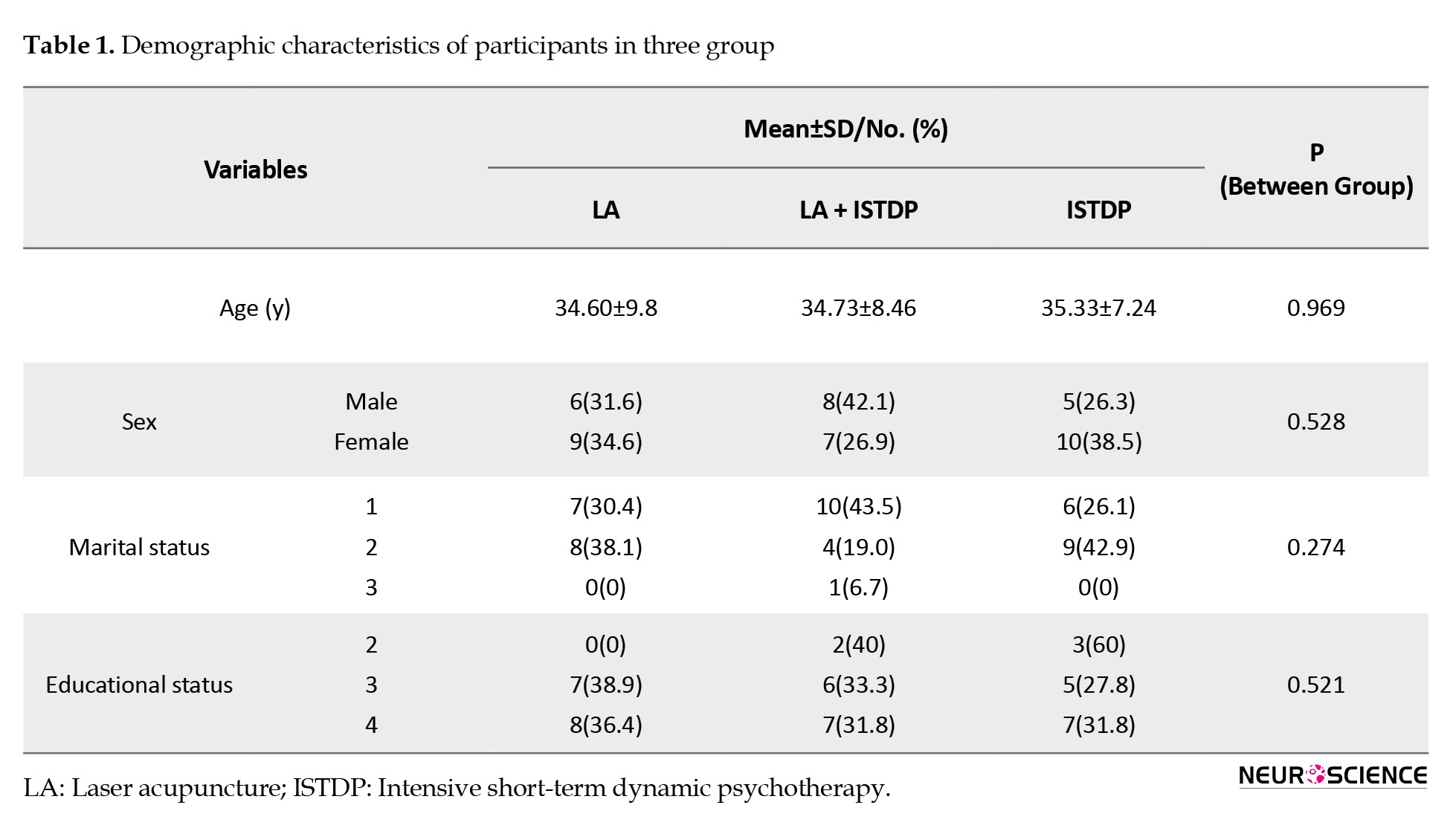
The mean age of the patients was 34.89±8.38 years. Regarding gender, 19 patients (42.2%) were male. All patients were seen and assessed at each time point.
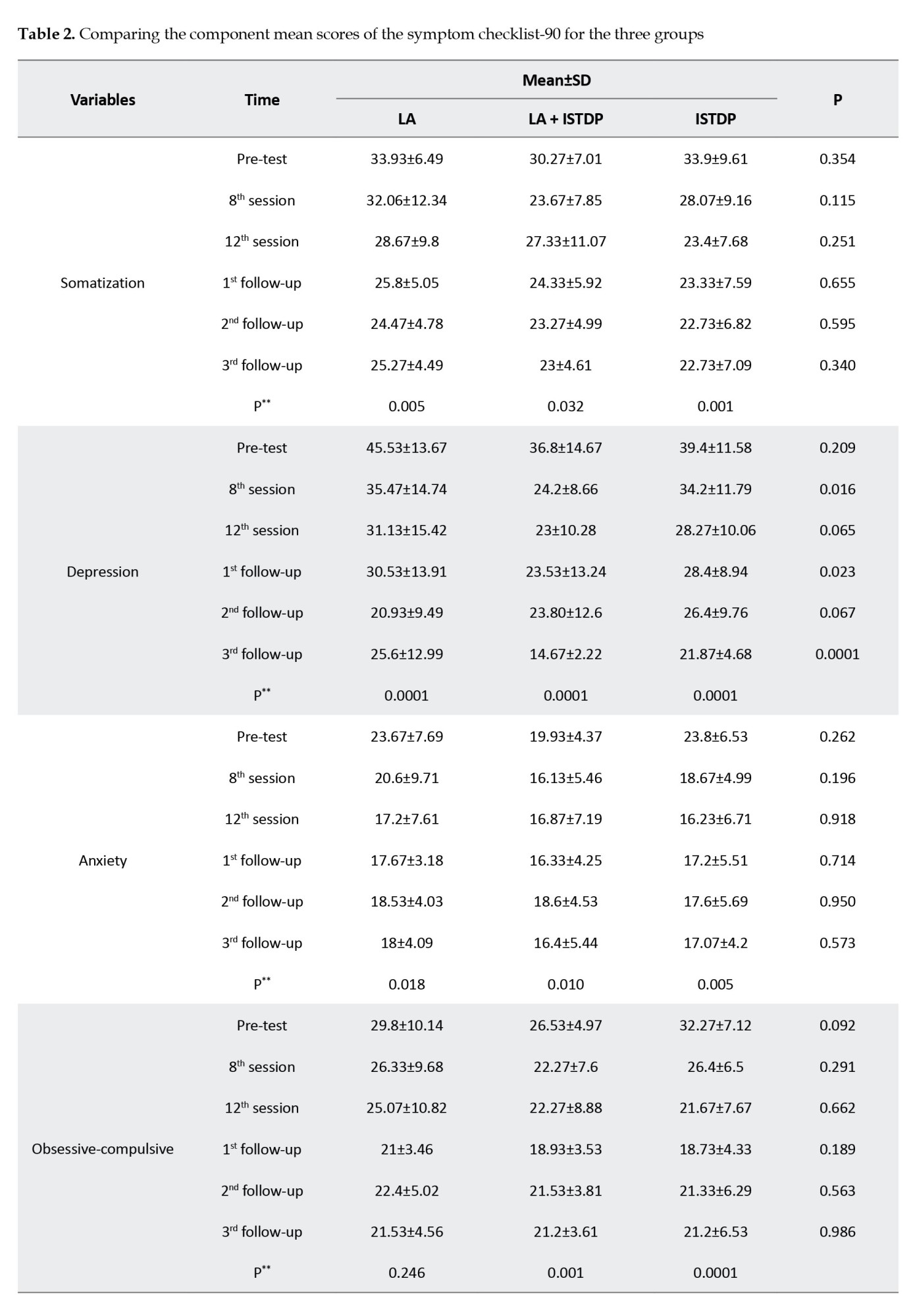
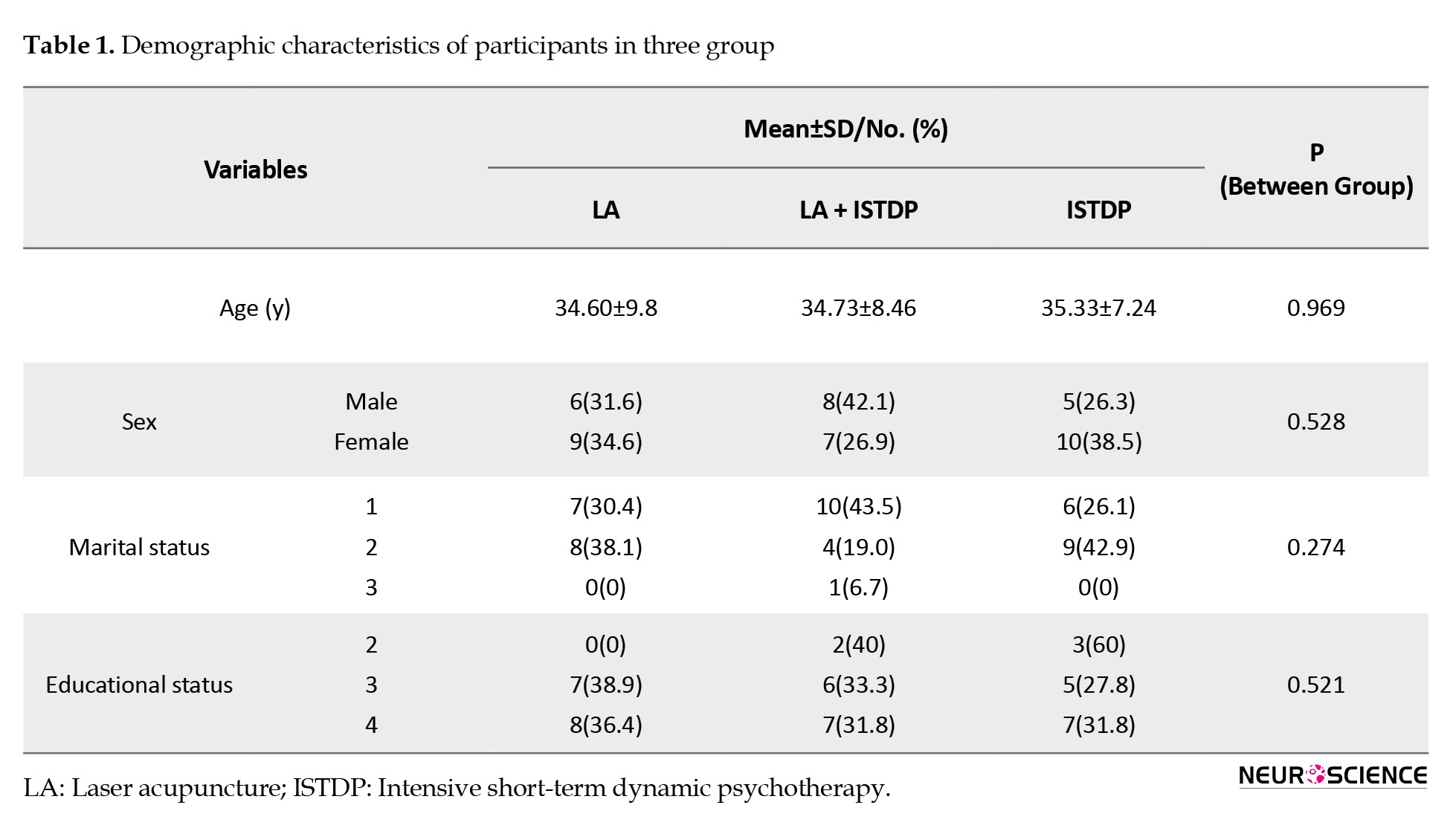
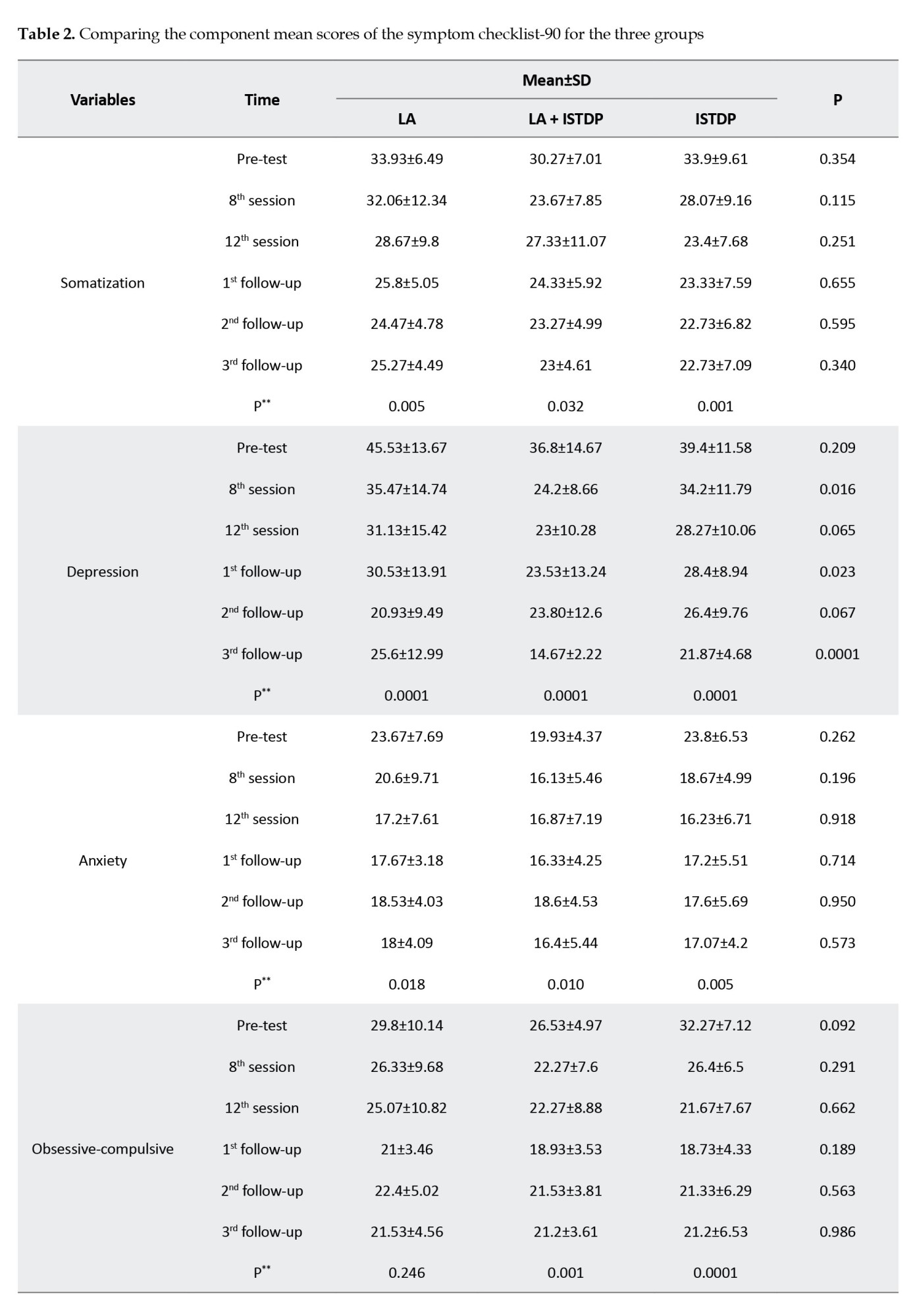
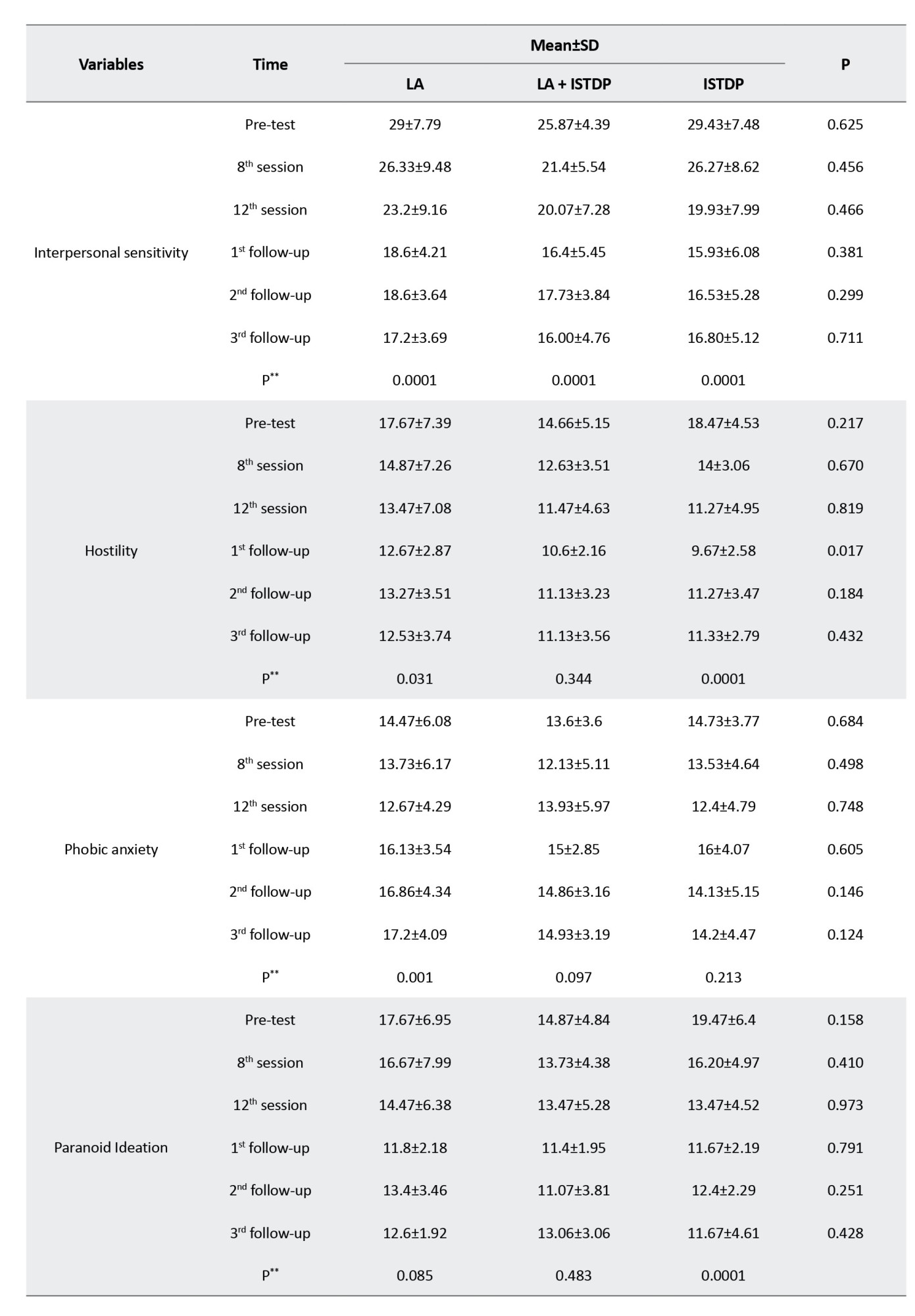
The results showed that in LA (1), LA with ISTDP (2), and ISTDP (3) groups, the HDRS (P=0.001, P=0.037, P<0.001, respectively), SCID (P<0.001, P<0.001, P=0.003, respectively) and SCL-90 (P<0.001, P<0.001, P<0.001, respectively) scores reduced over time within groups. HDRS scores at the eighth session and second follow-up in the LA with ISTDP group were lower than the LA group (P2, 1=0.010, P2, 1=0.011). However, the SCID score reduction was insignificant between the three groups. SCL-90 at the eighth session (P2, 3=0.014, P2, 1=0.011), first follow-up (P2, 3=0.018, P2, 1=0.017), and third follow-up in the LA with ISTDP group had the lowest score (P2, 3=0.001, P2, 1<0.001)
The subscales of the SCL-90, including somatization, depression, anxiety, obsessive-compulsive, interpersonal sensitivity, hostility, phobic anxiety, paranoid ideation, and psychoticism, were compared separately within each group over time, and each session was compared between three groups (Table 2).

4. Discussion
Using LA alone, ISTDP alone, and their combination effectively reduced depression on the main measure of HDRS. Regarding the SCL-90 depression subscale, all three groups also showed improvement, but this difference was greater in the third group at 2-time frames compared to the other two groups, suggesting that their combination may offer an advantage over either treatment alone. Although there were no baseline differences, the ISTDP alone group showed a marked and numerically much larger difference on the primary measure HDRS.
This study provides further evidence that ISTDP is an effective treatment for depression (Caldiroli et al., 2020). LA had a significant effect on reducing self-reported depression symptoms on the Beck depression scale (Quah-Smith et al., 2005) and HDRS in previous studies (Quah-Smith et al., 2013). The mean HDRS change was 9.28±6.55 in the previous study (Quah-Smith et al., 2013), while this measure evidenced a greater improvement in depressive symptoms in the current study. The results of this study regarding the combined effect of ISTDP and LA are also more robust and in a larger sample than the previous study. To add more, in this three-armed study, we designed a group with short-term intensive dynamic psychotherapy as a control group. However, the previous study evaluated LA therapy and LA combined with dynamic psychotherapy (Ghorbani et al., 2003).
LA may affect many structures and neurotransmitters in the central nervous system, including serotonin, norepinephrine, dopamine, and gamma-aminobutyric acid, as well as the hypothalamus, pituitary, thyroid, and adrenal glands (Quah-Smith et al., 2010; Spence et al., 2004; Xu, 2001). A study revealed the effect of LA on the brain of healthy individuals by brain functional magnetic resonance imaging, including LIV14, CV14, LIV8, and HT7, used in the treatment of depression on the activation of the frontal cortex, limbic and caudal cortex (Quah-Smith et al., 2010). At the same time, antidepressants work by modulating the subcortical frontal neural circuits (Goldapple et al., 2004).
The mechanism of LA and acupuncture is not well understood as a potential antidepressant treatment. Part of the antidepressant effect of this method may include default mode network modulation or resting-state network modulation (Gusnard & Raichle, 2001; Quah-Smith et al., 2013). Various mechanisms have been proposed for acupuncture, including stimulation of large peripheral nerves, neurovascular bundles, mechanical receptors, or free nerve terminals, but no anatomical neural structure or pathway has been established as a mediator of therapeutic effect (Napadow et al., 2008). Recent attention has been focused on the loss of intermuscular/intramuscular connective tissue, as many meridians and acupuncture points are aligned with this tissue (Langevin & Yandow, 2002). It has also been reported that acupuncture meridians have lower electrical impedance and higher capacitance than adjacent controls, which may justify using electrical acupuncture. Data are not conclusive (Ahn et al., 2008; Ahn et al., 2008); however, LA may prove to be an alternative approach to medication for treating depression.
Study limitations include the following five issues. First, unique cultural factors in Iran might affect recruitment, treatment expectations, and acceptance. All participants were Iranian; thus, there was no ethnic diversity within the recruited sample. Hence, these results may not be generalizable to other cultures. Second, as a single-blind RCT, therapists and patients could not be blinded to treatment allocations. Thus, outcomes could have been influenced by expectancy effects. Third, since two clinicians delivered the experimental treatments, it is unclear if the results are generalizable to other providers. Fourth, the likelihood of allegiance effects (Luborsky et al., 1999) may impact outcomes, although the blinded rating of depression on HDRS helps to offset this. Finally, the small sample size suggests further research should be done to test the relative efficacy of these treatments alone versus in combination.
5. Conclusion
ISTDP and LA appear to be effective treatments for major depression, with a possible added benefit from combining the two treatments. Future studies should include a larger study sample, comparative outcome study, and process-oriented design to understand how each of these two energy therapies affects the symptoms of depression.
Ethical Considerations
Compliance with ethical guidelines
The study protocol was registered with the Iranian Registry of Clinical Trial (IRCT) (Code: IRCT20111121008146N37) and approved by Shahid Beheshti Medical Science University Authority Research Ethics Board, Thran, Iran (Code: IR.SBMU.RETECH.REC.1396.1293).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization: Arista Shojaeddin; Methodology, software, validation, project administration, resources, and data curation: Arista Shojaeddin and Fariba Jafarian Namini; Investigation: Arista Shojaeddin, Nima Ghorbani, and Fariba Jafarian Namini; Formal analysis and visualization: Zahra Razzaghi; Writing the original draft: Arista Shojaeddin and Nima Ghorbani; Review and editing: Arista Shojaeddin, Nima Ghorbani and Allan Abbass; Supervision: Arista Shojaeddin and Nima Ghorbani;
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank the participants, research assistants, and all other staff of Insight-New Psychological Center in Tehran and the University of Tehran. The authors also especially thank Mansour Shamsipour for his helpful comments on randomization.
References
Abbass, A. (2015). Reaching through resistance: Advanced psychotherapy techniques. Kensington: Seven leaves press. [Link]
Abbass A. A. (2006). Intensive short-term dynamic psychotherapy of treatment-resistant depression: A pilot study. Depression and Anxiety, 23(7), 449–452. [DOI:10.1002/da.20203] [PMID]
Ahmadpanah, M., Sheikhbabaei, M., Haghighi, M., Roham, F., Jahangard, L., & Akhondi, A., et al. (2016). Validity and test-retest reliability of the Persian version of the Montgomery-Asberg Depression Rating Scale. Neuropsychiatric Disease and Treatment, 12, 603–607. [DOI:10.2147/NDT.S103869] [PMID]
Ahn, A. C., Colbert, A. P., Anderson, B. J., Martinsen, O. G., Hammerschlag, R., & Cina, S., et al. (2008). Electrical properties of acupuncture points and meridians: A systematic review. Bioelectromagnetics, 29(4), 245–256. [DOI:10.1002/bem.20403] [PMID]
Akhavan Abiri, F., & Shairi, M. R. (2020). [Validity and reliability of symptom checklist-90-revised (SCL-90-R) and brief symptom inventory-53 (BSI-53) (Persian)]. Clinical Psychology and Personality, 17(2), 169-195. [DOI:10.22070/cpap.2020.2916]
Ardakani, A., Seghatoleslam, T., Habil, H., Jameei, F., Rashid, R., & Zahirodin, A., et al. (2016). Construct validity of symptom checklist-90-revised (SCL-90-R) and general health questionnaire-28 (GHQ-28) in patients with drug addiction and diabetes, and normal population. Iranian Journal of Public Health, 45(4), 451–459. [PMID]
Armbrecht, E., Shah, A., Schepman, P., Shah, R., Pappadopulos, E., & Chambers, R., et al. (2020). Economic and humanistic burden associated with noncommunicable diseases among adults with depression and anxiety in the United States. Journal of Medical Economics, 23(9), 1032–1042. [DOI:10.1080/13696998.2020.1776297] [PMID]
Armour, M., Smith, C. A., Wang, L. Q., Naidoo, D., Yang, G. Y., & MacPherson, H., et al. (2019). Acupuncture for depression: A systematic review and meta-analysis. Journal of Clinical Medicine, 8(8), 1140. [DOI:10.3390/jcm8081140] [PMID]
Ay-Woan, P., Sarah, C. P., Lyinn, C., Tsyr-Jang, C., & Ping-Chuan, H. (2006). Quality of life in depression: Predictive models. Quality of Life Research, 15(1), 39–48. [DOI:10.1007/s11136-005-0381-x] [PMID]
Caldiroli, A., Capuzzi, E., Riva, I., Russo, S., Clerici, M., & Roustayan, C., et al. (2020). Efficacy of intensive short-term dynamic psychotherapy in mood disorders: A critical review. Journal of Affective Disorders, 273, 375–379. [DOI:10.1016/j.jad.2020.04.002] [PMID]
Dadfar, M., & Kalibatseva, Z. (2016). Psychometric properties of the Persian version of the short beck depression inventory with Iranian psychiatric outpatients. Scientifica, 2016, 8196463. [DOI:10.1155/2016/8196463] [PMID]
Fava, M., & Kendler, K. S. (2000). Major depressive disorder. Neuron, 28(2), 335–341. [DOI:10.1016/S0896-6273(00)00112-4] [PMID]
Ghassemzadeh, H., Mojtabai, R., Karamghadiri, N., & Ebrahimkhani, N. (2005). Psychometric properties of a Persian-language version of the beck depression inventory--second edition: BDI-II-PERSIAN. Depression and Anxiety, 21(4), 185–192. [DOI:10.1002/da.20070] [PMID]
Ghorbani, N., Watson, P., Bing, M. N., Davison, H. K., & LeBreton, D. (2003). Two facets of self-knowledge: Cross-cultural development of measures in Iran and the United States. Genetic, Social and General Psychology Monographs, 129(3), 238-268. [Link]
Ghorbani, N., Watson, P. J., & Hargis, M. B. (2008). Integrative Self-Knowledge Scale: Correlations and incremental validity of a cross-cultural measure developed in Iran and the United States. The Journal of Psychology, 142(4), 395–412. [DOI:10.3200/JRPL.142.4.395-412] [PMID]
Goldapple, K., Segal, Z., Garson, C., Lau, M., Bieling, P., & Kennedy, S., et al. (2004). Modulation of cortical-limbic pathways in major depression: Treatment-specific effects of cognitive behavior therapy. Archives of General Psychiatry, 61(1), 34–41. [DOI:10.1001/archpsyc.61.1.34] [PMID]
Gusnard, D. A., Raichle, M. E., & Raichle, M. E. (2001). Searching for a baseline: Functional imaging and the resting human brain. Nature reviews. Neuroscience, 2(10), 685–694. [DOI:10.1038/35094500] [PMID]
Husain, M. M., Rush, A. J., Fink, M., Knapp, R., Petrides, G., & Rummans, T., et al. (2004). Speed of response and remission in major depressive disorder with acute electroconvulsive therapy (ECT): A consortium for research in ECT (CORE) report. The Journal of Clinical Psychiatry, 65(4), 485–491. [DOI:10.4088/JCP.v65n0406] [PMID]
Hussenoeder, F. S., Jentzsch, D., Matschinger, H., Hinz, A., Kilian, R., & Riedel-Heller, S. G., et al. (2020). Depression and quality of life in old age: A closer look. European Journal of Ageing, 18(1), 75–83. [DOI:10.1007/s10433-020-00573-8] [PMID]
Khalkhali, H. R., Gharaaghaji, R., Ghojogh, M. G., & Valizadeh, R. (2018). Factors and prevalence of depression in students at Iran’s Urmia University of Medical Sciences. Internal Medicine and Medical Investigation Journal, 3(1), 12-16. [DOI:10.24200/imminv.v2i4.96]
Kubitz, N., Mehra, M., Potluri, R. C., Garg, N., & Cossrow, N. (2013). Characterization of treatment resistant depression episodes in a cohort of patients from a US commercial claims database. Plos One, 8(10), e76882. [DOI:10.1371/journal.pone.0076882] [PMID]
Kupfer, D. J., Frank, E., & Phillips, M. L. (2012). Major depressive disorder: New clinical, neurobiological, and treatment perspectives. Lancet, 379(9820), 1045–1055. [DOI:10.1016/S0140-6736(11)60602-8] [PMID]
Langevin, H. M., & Yandow, J. A. (2002). Relationship of acupuncture points and meridians to connective tissue planes. The Anatomical Record, 269(6), 257–265. [DOI:10.1002/ar.10185] [PMID]
Lépine, J. P., & Briley, M. (2011). The increasing burden of depression. Neuropsychiatric Disease and Treatment, 7(Suppl 1), 3–7. [DOI:10.2147/NDT.S19617] [PMID]
Luborsky, L., Diguer, L., Seligman, D. A., Rosenthal, R., Krause, E. D., & Johnson, S., et al. (1999). The researcher’s own therapy allegiances: A “wild card” in comparisons of treatment efficacy. Clinical Psychology, 6(1), 95-106. [DOI:10.1093/clipsy.6.1.95]
Napadow, V., Ahn, A., Longhurst, J., Lao, L., Stener-Victorin, E., & Harris, R., et al. (2008). The status and future of acupuncture mechanism research. Journal of Alternative and Complementary Medicine, 14(7), 861–869. [DOI:10.1089/acm.2008.SAR-3] [PMID]
Orsolini, L., Latini, R., Pompili, M., Serafini, G., Volpe, U., & Vellante, F., et al. (2020). Understanding the complex of suicide in depression: From research to clinics. Psychiatry Investigation, 17(3), 207–221. [DOI:10.30773/pi.2019.0171] [PMID]
Pilkington K. (2010). Anxiety, depression and acupuncture: A review of the clinical research. Autonomic Neuroscience, 157(1-2), 91–95. [DOI:10.1016/j.autneu.2010.04.002] [PMID]
Quah-Smith, I., Sachdev, P. S., Wen, W., Chen, X., & Williams, M. A. (2010). The brain effects of laser acupuncture in healthy individuals: An FMRI investigation. Plos One, 5(9), e12619. [DOI:10.1371/journal.pone.0012619] [PMID]
Quah-Smith, I., Smith, C., Crawford, J. D., & Russell, J. (2013). Laser acupuncture for depression: A randomised double blind controlled trial using low intensity laser intervention. Journal of Affective Disorders, 148(2-3), 179–187. [DOI:10.1016/j.jad.2012.11.058] [PMID]
Quah-Smith, J. I., Tang, W. M., & Russell, J. (2005). Laser acupuncture for mild to moderate depression in a primary care setting-A randomised controlled trial. Acupuncture in Medicine, 23(3), 103–111. [DOI:10.1136/aim.23.3.103] [PMID]
Smith, C. A., Armour, M., Lee, M. S., Wang, L. Q., & Hay, P. J. (2018). Acupuncture for depression. The Cochrane Database of Systematic Reviews, 3(3), CD004046. [DOI:10.1002/14651858.CD004046.pub4] [PMID]
Spence, D. W., Kayumov, L., Chen, A., Lowe, A., Jain, U., & Katzman, M. A., et al. (2004). Acupuncture increases nocturnal melatonin secretion and reduces insomnia and anxiety: A preliminary report. The Journal of Neuropsychiatry and Clinical Neurosciences, 16(1), 19–28. [DOI:10.1176/jnp.16.1.19] [PMID]
Taguchi, R., Sato, K., Adomi, S., Tanaka, N., Tamura, H., & Tamura, T. (2019). Acupuncture and laser acupuncture as treatments for emotional distress in infertile women in Japan. Medical Acupuncture, 31(6), 372–378. [DOI:10.1089/acu.2019.1344] [PMID]
Town, J. M., Abbass, A., Stride, C., & Bernier, D. (2017). A randomised controlled trial of intensive short-term dynamic psychotherapy for treatment resistant depression: The Halifax depression study. Journal of Affective Disorders, 214, 15–25.[DOI:10.1016/j.jad.2017.02.035] [PMID]
Town, J. M., Abbass, A., Stride, C., Nunes, A., Bernier, D., & Berrigan, P. (2020). Efficacy and cost-effectiveness of intensive short-term dynamic psychotherapy for treatment resistant depression: 18-month follow-up of the Halifax depression trial. Journal of Affective Disorders, 273, 194–202. [DOI:10.1016/j.jad.2020.04.035] [PMID]
Town, J. M., Falkenström, F., Abbass, A., & Stride, C. (2022). The anger-depression mechanism in dynamic therapy: Experiencing previously avoided anger positively predicts reduction in depression via working alliance and insight. Journal of Counseling Psychology, 69(3), 326–336. [DOI:10.1037/cou0000581] [PMID]
van der Watt, G., Laugharne, J., & Janca, A. (2008). Complementary and alternative medicine in the treatment of anxiety and depression. Current Opinion in Psychiatry, 21(1), 37–42. [DOI:10.1097/YCO.0b013e3282f2d814] [PMID]
Sharifi V, Asadi S M, Mohammadi M R, Amini H, Kaviani H, Semnani Y, et al. (2004). Reliability and feasibility of the persian version of the structured diagnostic interview for DSM-IV (SCID). Advances in Cognitive Sciences. 6 (1 & 2):10-22. [Link]
Xu X. (2001). Acupuncture in an outpatient clinic in China: A comparison with the use of acupuncture in North America. Southern Medical Journal, 94(8), 813–816. [DOI:10.1097/00007611-200108000-00012] [PMID]
The mean age of the patients was 34.89±8.38 years. Regarding gender, 19 patients (42.2%) were male. All patients were seen and assessed at each time point.
The results showed that in LA (1), LA with ISTDP (2), and ISTDP (3) groups, the HDRS (P=0.001, P=0.037, P<0.001, respectively), SCID (P<0.001, P<0.001, P=0.003, respectively) and SCL-90 (P<0.001, P<0.001, P<0.001, respectively) scores reduced over time within groups. HDRS scores at the eighth session and second follow-up in the LA with ISTDP group were lower than the LA group (P2, 1=0.010, P2, 1=0.011). However, the SCID score reduction was insignificant between the three groups. SCL-90 at the eighth session (P2, 3=0.014, P2, 1=0.011), first follow-up (P2, 3=0.018, P2, 1=0.017), and third follow-up in the LA with ISTDP group had the lowest score (P2, 3=0.001, P2, 1<0.001)
The subscales of the SCL-90, including somatization, depression, anxiety, obsessive-compulsive, interpersonal sensitivity, hostility, phobic anxiety, paranoid ideation, and psychoticism, were compared separately within each group over time, and each session was compared between three groups (Table 2).

4. Discussion
Using LA alone, ISTDP alone, and their combination effectively reduced depression on the main measure of HDRS. Regarding the SCL-90 depression subscale, all three groups also showed improvement, but this difference was greater in the third group at 2-time frames compared to the other two groups, suggesting that their combination may offer an advantage over either treatment alone. Although there were no baseline differences, the ISTDP alone group showed a marked and numerically much larger difference on the primary measure HDRS.
This study provides further evidence that ISTDP is an effective treatment for depression (Caldiroli et al., 2020). LA had a significant effect on reducing self-reported depression symptoms on the Beck depression scale (Quah-Smith et al., 2005) and HDRS in previous studies (Quah-Smith et al., 2013). The mean HDRS change was 9.28±6.55 in the previous study (Quah-Smith et al., 2013), while this measure evidenced a greater improvement in depressive symptoms in the current study. The results of this study regarding the combined effect of ISTDP and LA are also more robust and in a larger sample than the previous study. To add more, in this three-armed study, we designed a group with short-term intensive dynamic psychotherapy as a control group. However, the previous study evaluated LA therapy and LA combined with dynamic psychotherapy (Ghorbani et al., 2003).
LA may affect many structures and neurotransmitters in the central nervous system, including serotonin, norepinephrine, dopamine, and gamma-aminobutyric acid, as well as the hypothalamus, pituitary, thyroid, and adrenal glands (Quah-Smith et al., 2010; Spence et al., 2004; Xu, 2001). A study revealed the effect of LA on the brain of healthy individuals by brain functional magnetic resonance imaging, including LIV14, CV14, LIV8, and HT7, used in the treatment of depression on the activation of the frontal cortex, limbic and caudal cortex (Quah-Smith et al., 2010). At the same time, antidepressants work by modulating the subcortical frontal neural circuits (Goldapple et al., 2004).
The mechanism of LA and acupuncture is not well understood as a potential antidepressant treatment. Part of the antidepressant effect of this method may include default mode network modulation or resting-state network modulation (Gusnard & Raichle, 2001; Quah-Smith et al., 2013). Various mechanisms have been proposed for acupuncture, including stimulation of large peripheral nerves, neurovascular bundles, mechanical receptors, or free nerve terminals, but no anatomical neural structure or pathway has been established as a mediator of therapeutic effect (Napadow et al., 2008). Recent attention has been focused on the loss of intermuscular/intramuscular connective tissue, as many meridians and acupuncture points are aligned with this tissue (Langevin & Yandow, 2002). It has also been reported that acupuncture meridians have lower electrical impedance and higher capacitance than adjacent controls, which may justify using electrical acupuncture. Data are not conclusive (Ahn et al., 2008; Ahn et al., 2008); however, LA may prove to be an alternative approach to medication for treating depression.
Study limitations include the following five issues. First, unique cultural factors in Iran might affect recruitment, treatment expectations, and acceptance. All participants were Iranian; thus, there was no ethnic diversity within the recruited sample. Hence, these results may not be generalizable to other cultures. Second, as a single-blind RCT, therapists and patients could not be blinded to treatment allocations. Thus, outcomes could have been influenced by expectancy effects. Third, since two clinicians delivered the experimental treatments, it is unclear if the results are generalizable to other providers. Fourth, the likelihood of allegiance effects (Luborsky et al., 1999) may impact outcomes, although the blinded rating of depression on HDRS helps to offset this. Finally, the small sample size suggests further research should be done to test the relative efficacy of these treatments alone versus in combination.
5. Conclusion
ISTDP and LA appear to be effective treatments for major depression, with a possible added benefit from combining the two treatments. Future studies should include a larger study sample, comparative outcome study, and process-oriented design to understand how each of these two energy therapies affects the symptoms of depression.
Ethical Considerations
Compliance with ethical guidelines
The study protocol was registered with the Iranian Registry of Clinical Trial (IRCT) (Code: IRCT20111121008146N37) and approved by Shahid Beheshti Medical Science University Authority Research Ethics Board, Thran, Iran (Code: IR.SBMU.RETECH.REC.1396.1293).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization: Arista Shojaeddin; Methodology, software, validation, project administration, resources, and data curation: Arista Shojaeddin and Fariba Jafarian Namini; Investigation: Arista Shojaeddin, Nima Ghorbani, and Fariba Jafarian Namini; Formal analysis and visualization: Zahra Razzaghi; Writing the original draft: Arista Shojaeddin and Nima Ghorbani; Review and editing: Arista Shojaeddin, Nima Ghorbani and Allan Abbass; Supervision: Arista Shojaeddin and Nima Ghorbani;
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank the participants, research assistants, and all other staff of Insight-New Psychological Center in Tehran and the University of Tehran. The authors also especially thank Mansour Shamsipour for his helpful comments on randomization.
References
Abbass, A. (2015). Reaching through resistance: Advanced psychotherapy techniques. Kensington: Seven leaves press. [Link]
Abbass A. A. (2006). Intensive short-term dynamic psychotherapy of treatment-resistant depression: A pilot study. Depression and Anxiety, 23(7), 449–452. [DOI:10.1002/da.20203] [PMID]
Ahmadpanah, M., Sheikhbabaei, M., Haghighi, M., Roham, F., Jahangard, L., & Akhondi, A., et al. (2016). Validity and test-retest reliability of the Persian version of the Montgomery-Asberg Depression Rating Scale. Neuropsychiatric Disease and Treatment, 12, 603–607. [DOI:10.2147/NDT.S103869] [PMID]
Ahn, A. C., Colbert, A. P., Anderson, B. J., Martinsen, O. G., Hammerschlag, R., & Cina, S., et al. (2008). Electrical properties of acupuncture points and meridians: A systematic review. Bioelectromagnetics, 29(4), 245–256. [DOI:10.1002/bem.20403] [PMID]
Akhavan Abiri, F., & Shairi, M. R. (2020). [Validity and reliability of symptom checklist-90-revised (SCL-90-R) and brief symptom inventory-53 (BSI-53) (Persian)]. Clinical Psychology and Personality, 17(2), 169-195. [DOI:10.22070/cpap.2020.2916]
Ardakani, A., Seghatoleslam, T., Habil, H., Jameei, F., Rashid, R., & Zahirodin, A., et al. (2016). Construct validity of symptom checklist-90-revised (SCL-90-R) and general health questionnaire-28 (GHQ-28) in patients with drug addiction and diabetes, and normal population. Iranian Journal of Public Health, 45(4), 451–459. [PMID]
Armbrecht, E., Shah, A., Schepman, P., Shah, R., Pappadopulos, E., & Chambers, R., et al. (2020). Economic and humanistic burden associated with noncommunicable diseases among adults with depression and anxiety in the United States. Journal of Medical Economics, 23(9), 1032–1042. [DOI:10.1080/13696998.2020.1776297] [PMID]
Armour, M., Smith, C. A., Wang, L. Q., Naidoo, D., Yang, G. Y., & MacPherson, H., et al. (2019). Acupuncture for depression: A systematic review and meta-analysis. Journal of Clinical Medicine, 8(8), 1140. [DOI:10.3390/jcm8081140] [PMID]
Ay-Woan, P., Sarah, C. P., Lyinn, C., Tsyr-Jang, C., & Ping-Chuan, H. (2006). Quality of life in depression: Predictive models. Quality of Life Research, 15(1), 39–48. [DOI:10.1007/s11136-005-0381-x] [PMID]
Caldiroli, A., Capuzzi, E., Riva, I., Russo, S., Clerici, M., & Roustayan, C., et al. (2020). Efficacy of intensive short-term dynamic psychotherapy in mood disorders: A critical review. Journal of Affective Disorders, 273, 375–379. [DOI:10.1016/j.jad.2020.04.002] [PMID]
Dadfar, M., & Kalibatseva, Z. (2016). Psychometric properties of the Persian version of the short beck depression inventory with Iranian psychiatric outpatients. Scientifica, 2016, 8196463. [DOI:10.1155/2016/8196463] [PMID]
Fava, M., & Kendler, K. S. (2000). Major depressive disorder. Neuron, 28(2), 335–341. [DOI:10.1016/S0896-6273(00)00112-4] [PMID]
Ghassemzadeh, H., Mojtabai, R., Karamghadiri, N., & Ebrahimkhani, N. (2005). Psychometric properties of a Persian-language version of the beck depression inventory--second edition: BDI-II-PERSIAN. Depression and Anxiety, 21(4), 185–192. [DOI:10.1002/da.20070] [PMID]
Ghorbani, N., Watson, P., Bing, M. N., Davison, H. K., & LeBreton, D. (2003). Two facets of self-knowledge: Cross-cultural development of measures in Iran and the United States. Genetic, Social and General Psychology Monographs, 129(3), 238-268. [Link]
Ghorbani, N., Watson, P. J., & Hargis, M. B. (2008). Integrative Self-Knowledge Scale: Correlations and incremental validity of a cross-cultural measure developed in Iran and the United States. The Journal of Psychology, 142(4), 395–412. [DOI:10.3200/JRPL.142.4.395-412] [PMID]
Goldapple, K., Segal, Z., Garson, C., Lau, M., Bieling, P., & Kennedy, S., et al. (2004). Modulation of cortical-limbic pathways in major depression: Treatment-specific effects of cognitive behavior therapy. Archives of General Psychiatry, 61(1), 34–41. [DOI:10.1001/archpsyc.61.1.34] [PMID]
Gusnard, D. A., Raichle, M. E., & Raichle, M. E. (2001). Searching for a baseline: Functional imaging and the resting human brain. Nature reviews. Neuroscience, 2(10), 685–694. [DOI:10.1038/35094500] [PMID]
Husain, M. M., Rush, A. J., Fink, M., Knapp, R., Petrides, G., & Rummans, T., et al. (2004). Speed of response and remission in major depressive disorder with acute electroconvulsive therapy (ECT): A consortium for research in ECT (CORE) report. The Journal of Clinical Psychiatry, 65(4), 485–491. [DOI:10.4088/JCP.v65n0406] [PMID]
Hussenoeder, F. S., Jentzsch, D., Matschinger, H., Hinz, A., Kilian, R., & Riedel-Heller, S. G., et al. (2020). Depression and quality of life in old age: A closer look. European Journal of Ageing, 18(1), 75–83. [DOI:10.1007/s10433-020-00573-8] [PMID]
Khalkhali, H. R., Gharaaghaji, R., Ghojogh, M. G., & Valizadeh, R. (2018). Factors and prevalence of depression in students at Iran’s Urmia University of Medical Sciences. Internal Medicine and Medical Investigation Journal, 3(1), 12-16. [DOI:10.24200/imminv.v2i4.96]
Kubitz, N., Mehra, M., Potluri, R. C., Garg, N., & Cossrow, N. (2013). Characterization of treatment resistant depression episodes in a cohort of patients from a US commercial claims database. Plos One, 8(10), e76882. [DOI:10.1371/journal.pone.0076882] [PMID]
Kupfer, D. J., Frank, E., & Phillips, M. L. (2012). Major depressive disorder: New clinical, neurobiological, and treatment perspectives. Lancet, 379(9820), 1045–1055. [DOI:10.1016/S0140-6736(11)60602-8] [PMID]
Langevin, H. M., & Yandow, J. A. (2002). Relationship of acupuncture points and meridians to connective tissue planes. The Anatomical Record, 269(6), 257–265. [DOI:10.1002/ar.10185] [PMID]
Lépine, J. P., & Briley, M. (2011). The increasing burden of depression. Neuropsychiatric Disease and Treatment, 7(Suppl 1), 3–7. [DOI:10.2147/NDT.S19617] [PMID]
Luborsky, L., Diguer, L., Seligman, D. A., Rosenthal, R., Krause, E. D., & Johnson, S., et al. (1999). The researcher’s own therapy allegiances: A “wild card” in comparisons of treatment efficacy. Clinical Psychology, 6(1), 95-106. [DOI:10.1093/clipsy.6.1.95]
Napadow, V., Ahn, A., Longhurst, J., Lao, L., Stener-Victorin, E., & Harris, R., et al. (2008). The status and future of acupuncture mechanism research. Journal of Alternative and Complementary Medicine, 14(7), 861–869. [DOI:10.1089/acm.2008.SAR-3] [PMID]
Orsolini, L., Latini, R., Pompili, M., Serafini, G., Volpe, U., & Vellante, F., et al. (2020). Understanding the complex of suicide in depression: From research to clinics. Psychiatry Investigation, 17(3), 207–221. [DOI:10.30773/pi.2019.0171] [PMID]
Pilkington K. (2010). Anxiety, depression and acupuncture: A review of the clinical research. Autonomic Neuroscience, 157(1-2), 91–95. [DOI:10.1016/j.autneu.2010.04.002] [PMID]
Quah-Smith, I., Sachdev, P. S., Wen, W., Chen, X., & Williams, M. A. (2010). The brain effects of laser acupuncture in healthy individuals: An FMRI investigation. Plos One, 5(9), e12619. [DOI:10.1371/journal.pone.0012619] [PMID]
Quah-Smith, I., Smith, C., Crawford, J. D., & Russell, J. (2013). Laser acupuncture for depression: A randomised double blind controlled trial using low intensity laser intervention. Journal of Affective Disorders, 148(2-3), 179–187. [DOI:10.1016/j.jad.2012.11.058] [PMID]
Quah-Smith, J. I., Tang, W. M., & Russell, J. (2005). Laser acupuncture for mild to moderate depression in a primary care setting-A randomised controlled trial. Acupuncture in Medicine, 23(3), 103–111. [DOI:10.1136/aim.23.3.103] [PMID]
Smith, C. A., Armour, M., Lee, M. S., Wang, L. Q., & Hay, P. J. (2018). Acupuncture for depression. The Cochrane Database of Systematic Reviews, 3(3), CD004046. [DOI:10.1002/14651858.CD004046.pub4] [PMID]
Spence, D. W., Kayumov, L., Chen, A., Lowe, A., Jain, U., & Katzman, M. A., et al. (2004). Acupuncture increases nocturnal melatonin secretion and reduces insomnia and anxiety: A preliminary report. The Journal of Neuropsychiatry and Clinical Neurosciences, 16(1), 19–28. [DOI:10.1176/jnp.16.1.19] [PMID]
Taguchi, R., Sato, K., Adomi, S., Tanaka, N., Tamura, H., & Tamura, T. (2019). Acupuncture and laser acupuncture as treatments for emotional distress in infertile women in Japan. Medical Acupuncture, 31(6), 372–378. [DOI:10.1089/acu.2019.1344] [PMID]
Town, J. M., Abbass, A., Stride, C., & Bernier, D. (2017). A randomised controlled trial of intensive short-term dynamic psychotherapy for treatment resistant depression: The Halifax depression study. Journal of Affective Disorders, 214, 15–25.[DOI:10.1016/j.jad.2017.02.035] [PMID]
Town, J. M., Abbass, A., Stride, C., Nunes, A., Bernier, D., & Berrigan, P. (2020). Efficacy and cost-effectiveness of intensive short-term dynamic psychotherapy for treatment resistant depression: 18-month follow-up of the Halifax depression trial. Journal of Affective Disorders, 273, 194–202. [DOI:10.1016/j.jad.2020.04.035] [PMID]
Town, J. M., Falkenström, F., Abbass, A., & Stride, C. (2022). The anger-depression mechanism in dynamic therapy: Experiencing previously avoided anger positively predicts reduction in depression via working alliance and insight. Journal of Counseling Psychology, 69(3), 326–336. [DOI:10.1037/cou0000581] [PMID]
van der Watt, G., Laugharne, J., & Janca, A. (2008). Complementary and alternative medicine in the treatment of anxiety and depression. Current Opinion in Psychiatry, 21(1), 37–42. [DOI:10.1097/YCO.0b013e3282f2d814] [PMID]
Sharifi V, Asadi S M, Mohammadi M R, Amini H, Kaviani H, Semnani Y, et al. (2004). Reliability and feasibility of the persian version of the structured diagnostic interview for DSM-IV (SCID). Advances in Cognitive Sciences. 6 (1 & 2):10-22. [Link]
Xu X. (2001). Acupuncture in an outpatient clinic in China: A comparison with the use of acupuncture in North America. Southern Medical Journal, 94(8), 813–816. [DOI:10.1097/00007611-200108000-00012] [PMID]
Type of Study: Original |
Subject:
Behavioral Neuroscience
Received: 2023/11/19 | Accepted: 2024/04/15 | Published: 2025/01/1
Received: 2023/11/19 | Accepted: 2024/04/15 | Published: 2025/01/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |