Volume 12, Issue 4 (July & August 2021)
BCN 2021, 12(4): 477-488 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Modarres Zadeh A, Mehri A, Jalaei S, Khatoonabadi A R, Kalbe E. Translation and Cross-cultural Adaptation of the Aphasia Check List in Persian Speakers With Aphasia. BCN 2021; 12 (4) :477-488
URL: http://bcn.iums.ac.ir/article-1-1534-en.html
URL: http://bcn.iums.ac.ir/article-1-1534-en.html
Translation and Cross-cultural Adaptation of the Aphasia Check List in Persian Speakers With Aphasia
1- Department of Speech and Language Pathology, School of Rehabilitation Sciences, Tehran University of Medical Sciences, Tehran, Iran.
2- Department of Physical Sciences, School of Rehabilitation Sciences, Tehran University of Medical Sciences, Tehran, Iran.
3- Medizinische Psychologie Neuropsychologie und Gender Studies, Centrum Für Neuropsychologische Diagnostik und Intervention (CeNDI), Prodekanin Für Akademische Entwicklung and Gender, Köln, Germany.
2- Department of Physical Sciences, School of Rehabilitation Sciences, Tehran University of Medical Sciences, Tehran, Iran.
3- Medizinische Psychologie Neuropsychologie und Gender Studies, Centrum Für Neuropsychologische Diagnostik und Intervention (CeNDI), Prodekanin Für Akademische Entwicklung and Gender, Köln, Germany.
Full-Text [PDF 1634 kb]
| Abstract (HTML)
Full-Text:
1. Introduction
Aphasia is an acquired disorder of verbal communication. It always occurs due to some damage to certain parts of the brain responsible for speech and language processing. It is mainly manifested by impairments in the receptive and expressive modalities of spoken and written language to different extents (Hallowell & Chapey, 2008). Moreover, the deficits of memory (Vallila-Rohter & Kiran, 2013; Mayer & Murray, 2012), attention (Murray, 2012; Villard & Kiran), reasoning (Murray, 2012), and executive functions (Murray, 2017) can be comorbid with aphasia. Cerebrovascular accident is the most prevalent cause of aphasia. Ischemic infarction causes 80% of aphasic cases (Berthier, 2005). According to the studies conducted in Europe and the US, one-third of all patients with stroke are prone to aphasia in acute stages (Damico, Müller & Ball, 2010; Engelter et al., 2006; Laska, Hellborn, Murray, Kahan, & Von Arbin, 2001). In Iran, two studies examined the prevalence of aphasia. A cross-sectional study indicated that 5 out of 22 stroke patients (equal to 22.7% of the statistical population) had aphasia (Soltani, Khatoonabadi, Jenabi, & Piran, 2013). A retrospective study revealed that 727 out of 1817 such patients (equal to 39.9% of the statistical population) had a particular type of aphasia (Zamani & Madjdinasab, 2013). The relatively high prevalence of aphasia among patients with a first-ever stroke adversely affects the affected individuals’ quality of life respecting depression and social isolation (Kauhanen et al., 2000; Davidson, Howe, Worrall, Hickson, & Togher, 2008). Thus, it seems necessary to implement early intervention programs (Godecke et al., 2014); the first step of which is evaluation (Papathanasiou, Coppens, & Potagas, 2012). Evaluation can be conducted for various purposes as determining the presence of aphasia and its classification; the severity of the disorder; the nature of the observed language disorders; setting therapeutic objectives and adopting adequate approaches; treatment prognosis, and changes in the treatment process (Bruce & Edmundson, 2010). One aphasia test alone cannot meet all of the above-mentioned goals. Therefore, clinicians were advised to reflect on the exact purpose of their examination before choosing assessment tools (Spreen & Risser, 2003). When a therapist intends to collect samples from various verbal behaviors at different levels of assignment difficulty in the expressive and receptive modalities, comprehensive aphasia tests should be used (Patterson & Chapey, 2008).
The Persian Aphasia Test is the only comprehensive scale released in Iran. It evaluates the 6 primary language skills, i.e., oral expression, oral comprehension, repetition, available vocabulary, reading, and writing. According to the developers, this test was used by speech and language pathologists for over 20 years within the country; however, its use may cause problems. This test consists of 25 subtests and 217 items. Thus, it might be time-consuming and tiring when conducted on an aphasic population because aphasia occurs mostly after the age of 65 years (Benjamin et al., 2017). Accordingly, patients may not be cooperative. As discussed earlier, aphasia is a multifaceted disorder that can affect other language-dependent aspects of cognitive functioning, such as non-word processing (Luzzatti, Toraldo, Zonca, Cattani, & Saletta, 2006), numerical processing (Delazer & Bartha, 2001), and neuropsychological abilities including memory, attention, and reasoning (Murray, 2012; El Hachioui et al., 2014). Therefore, a comprehensive aphasia test should also cover these areas. Accordingly, the authors of this paper decided to translate the ACL, i.e., a German aphasia test, and evaluate its psychometric features. The ACL has certain advantages, the most important of which is that it takes 30-40 minutes to administer the entire test. This feature enables the therapist to finish the evaluation process in one session; therefore, respondents will experience less fatigue. Another feature of this test is that it uses various verbal stimuli [sentences, words (nouns & verbs), non-words, & numbers] for language evaluation. These stimuli become systematically complicated every task, something which can significantly help in pinpointing the examinee’s level of performance. Moreover, to minimize the interference of a faulty language system during the cognitive assessment, nonverbal stimuli were used in the cognition part of the test (Kalbe, Reinhold, Brand, Markowitsch, & Kessler, 2005). This test was provided with cut-off points per subtest in the language and cognition sections to evaluate the presence of disorder in the respective area of functioning; also a total cut-off point is determined for determining the presence of aphasia in the language section. It is easy to conduct and has a convenient scoring method. Therefore, it appeared that translating and publishing this test could greatly help Iranian therapists to increase the quality of intervention offered to PWA.
2. Methods
Initially, permission to translate the test to Persian was obtained from the test developer. Then, the translation process began based on the International Quality of Life Assessment (IQOLA) protocol for standard translation (Ware & Gandek, 1998).
Phase 1: The German-to-Persian translation process was started by two Persian-speaking translators (Translator 1 and Translator 2). These two translators mastered languages and linguistics terms and concepts. However, they were unfamiliar with the ACL test, and each one independently translated the test.
Phase 2: After finishing the forward translation process, each translator was requested to score all sections translated by the other translator (words, expressions, & sentences) concerning difficulty using a 100-point Likert-type scale, in which 0 indicate completely understandable, and 100 reflect unintelligibly. If an item was scored above 30, it would be considered hard, then returned to its translator. In this section, none of the items was scored above 30.
Phase 3: In this phase, two other bilingual translators were requested to score the quality of each version of the translations. By quality, we mean the simplicity and clarity of translation. These translators had no connection to translators 1 and 2 and lacked clinical experience. They independently gave scores from each other. Again, a 100-point visual scale was employed. On this scale, 0 addressed the lowest quality of translation, and 100 indicated the highest. With a score <90, the translation was considered low-quality with the need for revision by its translator. In this phase, none of the items received a score below 90.
Phase 4: In this phase, an expert panel was held for translators 1 and 2, and the researchers to evaluate and compare the difficulty and quality of the translations. At last, one translation was agreed upon.
Phase 5: The final translated version of the ACL in Persian was back-translated by another translator (translator 5) into German. This translator had not been present in the previous phases and knew nothing about the purpose and intended use of the ACL.
Phase 6: After finishing the back-translation, the original version of the test was compared with the back-translated version by an expert panel for any necessary corrections or revisions. Finally, a satisfactory Persian version of the text was reached.
Phase 7: Ten speech and language pathologists working in the field of aphasia management were requested to score the pre-final Persian version concerning its following the required criteria using a 4-point Likert-type scale respecting the comprehensibility of the commands and stimuli; the sociocultural suitability of the test stimuli; and the clarity and fluency of the used words, expressions, and sentences. On this scale, 0 reflected the absence of the criteria as mentioned earlier, and 4 reflected full compliance with them. If 80% of the respondents gave <3 to any item, it had to be sent to the corresponding translator for revision. All of the verbal items received acceptable scores. The expert panel confirmed the adequacy of the results of this field testing, and the Persian version of the ACL (called ACL-P from now on) was prepared to be evaluated among a population of PWA.
In this study, the required PWAs were recruited based on the following criteria from the caseload of clinics affiliated with Tehran University of Medical Sciences through the convenience sampling method. The inclusion criteria were a first left-hemisphere stroke caused aphasia, and there had been no other previous strokes; at least 3months had passed since the stroke before the initiation of the study; the maximum age of 65 years; the native language had to be Persian, and the participant had to be literate before the occurrence of the lesion; no comorbid neurodegenerative or psychiatric diseases (e.g., dementia of Alzheimer’s type or clinical depression) based on their medical history, their prescribed medications and caregivers’ reports of their problems; participants had not received speech/language interventions at least one week before the testing sessions (they had already completed a program or were awaiting to be enrolled in a new program, or for whatever reason did not intend to take part in the speech therapy facilities available to them.
However, if they were receiving any program, they were excluded from this study. In addition to the usual evaluations of speech therapy, an experienced neurologist was available to confirm the diagnosis of aphasia. Neurologically, healthy controls were selected from the clients referred to the same clinics. They were the caretakers of participant patients or had other complaints than speech and language disorders (e.g., optometric & lower-back problems). The inclusion criteria for healthy participants were no history of verbal or cognitive disorders (diagnosed through the Persian version of MMSE; cut-off point= 23) (Seyedian et al., 2008); the lack of any biopsychological disorders disrupting test implementation; Persian as their native language (or using Persian as their preferred language in case of being bi/multilingual); being adequately literate to meet daily needs.
The research goals were explained to all study participant and their caretakers. Then, they were requested to sign an informed written consent, i.e., securely stored by one of the researchers.
The ACL-P was individually provided to the research participant. The test was conducted in an acoustic well-lit room at the Rehabilitation School of Tehran University of Medical Sciences, away from any visual distractions. If a participant could not attend this location for any reason, the testing sessions were pursued at their home per standard conditions. The language learning section was implemented by asking oral questions or showing pictures/printed words and recording responses. The cognitive section was paper-based. The study participants had to cross out the target items in the attention subtest. Moreover, PWAs used their non-dominant left hands to complete the task. Thus, before implementing the test in this group, they practiced crossing out geometrical items, such as squares and triangles with pencils to concentrate on the test instead of figuring out how to complete the task. The oral responses were immediately transcribed. However, these responses were also recorded by a device (Sony SO-ICD-PX240 4GB Voice Recorder). The retest session was held 10 days after the first testing session per study participant by the same examiner in the same conditions.
The ACL-P consists of two general sections; language and cognition. The language section consists of the following 7 subtests, used to evaluate the primary modalities of verbal comprehension and expression, reading, writing, and repetition, as follows: serial speech (2 tasks); following commands (2 tasks); the color-shape test; word generation (2 tasks); specific verbal abilities: a) confrontation naming; b) reading aloud; c) reading comprehension; d) listening comprehension; e) writing to dictation; f) repetition (45 tasks); evaluation of general verbal communication ability, and numerical processing (3 tasks). The cognitive section consists of 3 subtests i.e., memory, attention, and reasoning. Regarding the memory subtest, the participants looked at 6 geometrical shapes for 10 seconds. Then, they were requested to recognize them among an assortment of shapes immediately (short-term memory) and after 10 minutes (mid-term memory). The attention section was designed to evaluate the speed and quality of selective attention through a task of canceling out two geometrical shapes in a block of similar shapes. Regarding reasoning, there were 11 sequences of 9 objects, 8 of which were arranged according to a rule, and the examiner must determine the one that disrupted the arrangement (Kalbe et al., 2005).
The resultant data were analyzed in SPSS. The Shapiro-Wilk test was conducted to check the normality of data. The Mann-Whitney U test was performed to evaluate the discriminant validity. The ICC coefficients (an absolute agreement, two-way mixed) were employed to determine the test-retest reliability of the scale. The lowest acceptable coefficient was considered 0.5, and values ranging between 0.5 and 0.75, between 0.75 and 0.9, and over 0.9 were respectively considered mediocre, good, and excellent. Cronbach’s alpha coefficient was employed to analyze the internal consistency of the scale. The coefficients ranging between 0.7 and 0.9 were regarded as excellent. The Spearman rank correlation coefficient test was implemented to determine the correlation between the language and cognition parts of the test. The minimum and maximum scores were considered to determine the floor and ceiling effects, respectively. The floor and ceiling effects were significant if they were observed to be over 15%.
3. Results
In this study, the statistical population included 20 PWA (13 males & 7 females with the Mean±SD age of 56.90±7.51 years & the age range of 45-65 years) and 50 neurologically healthy individuals (29 males & 21 females with the Mean±SD age of 59.80±5.20 years and the age range of 52-70 years). The Mean±SD years of education in the patient and control groups were 11.85±3.94 years (range: 5-18 years) and 11.34±3.79 years (range: 4-18 years). According to the Shapiro-Wilk test results, age followed no normal distribution in the patient group (W= 0.864 & P= 0.009) and the control group (W= 0.939 & P= 0.013). The educational attainment had a normal distribution in the patient group (W= 0.905 & P= 0.052); however, it suggested a significant difference from the normal distribution in the control group (W= 0.906 & P= 0.001). There was no significant difference between the study groups concerning age (U= 408 & P= 0.230) and education (U= 455 & P= 0.543). The Mean±SD score of the elapsed time from the onset of the disorder to the initiation of the study was measured as 29.7±17.89 months, with a range of 8-60 months in the patient group. Based on hospital discharge records, MRI scans, and language evaluations via the P-WAB-1 test (Nilipour, Pourshahbaz, & Ghoryshi, 2014), the type of aphasia was categorized in all the subjects as non-fluent. It was due to lesions to the perisylvian areas of the left hemisphere. In the control group, the MMSE test was conducted to evaluate mental health. Their Mean±SD scores were 27.76±2.20, with a range of 24-30.
The total scores of all language assignments of the ACL-P were 213. For the language section of the test, the means and ranges of the total scores in the test (Mean±SD= 112.7±7.58 & range= 63-171) and retest (Mean±SD= 120.35±7.20 & range= 69-174) sessions reflected no floor and ceiling effects. The distribution of scores was normal in the patient group in the test (W= 0.935 & P= 0.191) and the retest (W= 0.952 & P= 395) phases. According to the test’s manual, 8 subtests (phonological fluency, semantic fluency, listening comprehension, reading comprehension, naming, reading aloud, the dictation of words & sentences, the repetition of words & sentences, & color-shape test) were considered the essential subtests (these subtests are henceforth called diagnostic subtests). The maximum total score for these subtests was 148. The scores of the patient group presented no such effects in the test (Mean±SD= 78.10±24.01; range=44-115) and the retest (Mean±SD= 82.5±22.75; range=42-120) for the diagnostic subtests. The distribution of scores was normal in the test (W= 907 & P= 0.56) and the retest (W= 0.952 & P= 0.395). Given that the constructs are dependent on each other in the cognition part of the ACL-P, the scores of this section cannot be added together.
Therefore, each subtest’s score was reported separately for this part of the test. No floor and ceiling effects were observed for immediate memory (mean=4.45; range= -1 to 6) in the test and in the retest sessions (mean= 4.95; range= 3-6); also the case for delayed memory in the test (mean= 3.95; range= 2-6) and the retest (mean= 4.3; range= 2-6) sessions (the minimum score was -6 on this subtest). In the attention section, 3 scores were determined: the total number of processed items (144 at most), the differentiation of the processed items and errors (no maximum), and error frequency (66.6% at most). There were no floor and ceiling effects either for the total number of processed items in the test (mean= 61; range= 25-117) or the retest (mean= 56.5; range=24-110) nor were there any for the error percentage in the test (mean= 5.14; range= 0-22.2) and the retest (mean= 5.07; range= 0-15.6) sessions. Regarding the subtest of reasoning (the maximum score equaled 11), the same was true in the test (mean= 5.8, range= 4-10) and the retest (mean= 6; range= 4-10) sessions. The next section addresses the floor and ceiling effects on each subtest.
There were significant differences between the total score of the language section (Mann–Whitney U= 6.000, n1= 50, n2= 20, P<0.001) and the scores of diagnostic subtests (Mann–Whitney U=3.000, n1= 50, n2= 20, P<0.001) for the control and PWA groups. Table 1 presents the control and patient scores on each subtest of the ACL-P in the first execution of the test.
.png)
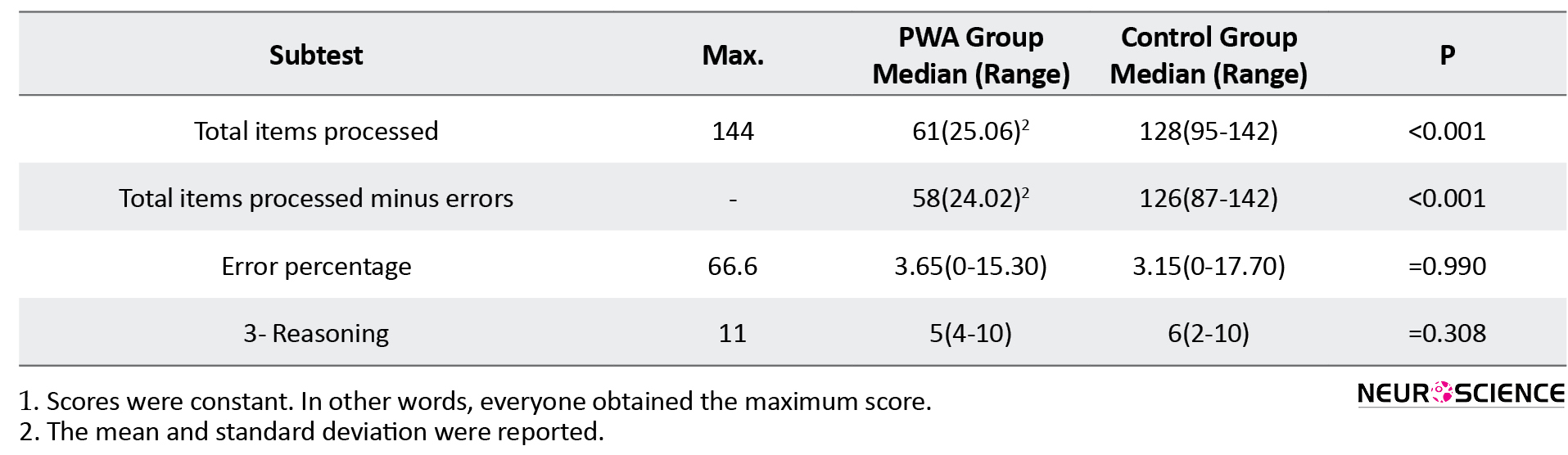
It also outlines the significance of the difference between the mean or median scores of these two groups. The results of most of these subtests did not follow a normal distribution in the patient and control groups; thus, the medians and score ranges were reported. If the scores follow a normal distribution, the mean and standard deviation are reported and highlighted. Accordingly, the research groups were significantly different from each other on all subtests of the language section. In the second section of the test, a significant difference was only observed in the subtest of attention. Cronbach’s alpha coefficient method was employed to test the internal consistency. The obtained coefficient was 0.761 for the entire test (both language and cognition sections were considered) in both test and retest phases. The values of Cronbach’s alpha coefficient ranged from 0.777 to 0.804 in the test phase and from 0.727 to 0.895 in the retest phase in case of item deletion. Cronbach’s alpha coefficient was calculated as 0.884 (ranged, if item deleted, from 0.867 to 0.884) for the language part and was measured to be 0.071 (ranged, if item deleted, from 0.060 to 0.563) for the cognition part in the test phase. These values were 0.899 (range= 0.878-904) for the language part and 0.120 (range= 0.052-0.123) for the cognition part in the retest. Regarding the diagnostic subtests of the language section, Cronbach’s alpha coefficient was computed as 0.852 in the test phase. However, it equaled 0.878 in the retest phase. If items were deleted, the coefficient ranged from 0.809 to 0.859 in the test phase and from 0.838 to 0.898 in the retest phase.
The value of ICCagreement was high for the total scores of the language section (ICC agreement= 0.982, 95%CI= 0.819-0.995, P<0.001). It was also high in the diagnostic subtests (ICCagreement= 0.981, 95%CI= 0.863-0.995, P<0.001). Table 2 manifests the values of ICCagreement determined for every ACL subtest in the language and cognition sections.
.png)
Accordingly, ICC was acceptable with a 95% confidence interval in all ACL-P subtests. More precisely, it ranged between 0.573 and 0.984 at a significance level of P<0.05.
As discussed earlier, the ACL-P test consists of two sections; language and cognition. According to the cognition part data, all of the surveyed patients had dysfunctions in at least one of the cognitive areas [short memory, midterm memory, attention (the total processed items minus errors), and reasoning]. A Performance lower than the cut-off points was observed in 4 participants on one subtest, in 9 participants on two subtests, in 3 participants on three subtests, and 4 participants on four subtests. The frequency of the presence of disorder in each domain was as follows: attention (19 participants), reasoning (15 participants), short-term memory (7 participants), and midterm memory (6 participants). Moreover, Table 3 indicates the values of correlation between the essential subtests of the language section and the subtests of the cognition section in the healthy and aphasic groups.
.png)
Accordingly, the number of significant correlations in the control group was more extensive than that of the PWA group. In the control group, the only subtest without correlations with the cognition subtests was repetition. In the patient group, the color-shape and repetition subtests had no correlations with any of the cognition subtests. The subtest of attention had the most significant number of correlations with the language subtests.
4. Discussion
This study aimed at the cultural adaptation and determination of the psychometric features of the ACL-P test. Accordingly, it could be used for evaluation purposes in Persian-speaking clinical environments where persons with aphasia attend. The coverage of a wide variety of language skills and the relatively short administration time make this test suitable for a time-saving but comprehensive assessment. The subtests include different numbers of tasks proportional to their relevance to the main characteristics of aphasia. For instance, the subtest for comprehension of words/sentences (i.e., essential for diagnosis and classification of aphasia syndromes) consisted of 6 tasks. In contrast, the subtest for reading numbers included three assignments. As a result, the therapist can screen lesser-important language skills and conduct a more comprehensive evaluation of these skills, only if it becomes necessary. The presence of nonverbal assignments for assessing short-term memory, midterm memory, attention, and reasoning are among the other hallmarks of this test. According to recent studies, cognitive functions can affect the evaluation process and the response to treatment. Therefore, it is essential to understand a patient’s cognitive status (Villard & Kiran, 2015).
The translation process was performed smoothly because a standard protocol was employed for translation. Furthermore, the stimuli and guidelines in the source language (German) were void of any linguistic complexity (e.g., the usage of words with multiple meanings or long sentences); the face and content validities of the test was appropriate. However, a few changes were made in the verbal stimuli of the test and pictures. As for the reading, repeating, and writing of non-words, the test items matching the Persian phonotactic constraints were used. The pictures used for naming and reading comprehension were changed to match the Islamic culture governing Iran (Figure 1).
.png)
Moreover, all of the other items matched the Persian language and Iranian culture.
As a group, the study participants with aphasia did not obtain the minimum and maximum scores in any subtest of ACL-P during the test and retest sessions. The analysis of every subtest of the language section found that several participants in the aphasia group did obtain maximum scores in the subtests of automatic speech, following commands, and numerical processing in the test and retest phases. One reason could be the type of aphasia. Auditory comprehension is usually damaged less than other language functions in nonfluent aphasia. This was the type presented by all aphasic patients in the current study; therefore, the maximum score was observed in the direction-following subtest. The satisfactory performance of some aphasic participants in the automatic speech subtest (including reciting the days of the week & counting to 15) was consistent with the fact that PWA presents better performances in non-propositional (automatic) language than in propositional language assignments (Lum & Ellis, 1999). Regarding the maximum score of the numerical processing subtests, the collected results were consistent with the evidence that there can be distinctions between verbal functions and numerical processing functions of aphasic patients (Rossor, Warrington, & Cipolotti, 1995). In the original paper introducing this test, the score range of reading, writing, and repeating numbers were between 0 and 9, indicating that some patients with the disorder may reach the maximum score in these subtests (Kalbe et al., 2005).
According to the Cronbach alpha coefficients of all subtests and diagnostic subtests, the ACL-P had an acceptable internal consistency. In the original paper of the test, the values of Cronbach’s alpha coefficient were reported to range between 0.4 and 0.88 (Kalbe et al., 2005). Lower internal consistency of the cognition part of the ACL-P, compared to that of the language part, was expected. This is because it consisted of distinct cognitive domains of memory, attention, and reasoning (Sachdev et al., 2014). Moreover, this test demonstrated acceptable test-retest reliability. In the original normative study of the ACL, the test-retest reliability ranged between 0.5 and 0.91 at P<0.05; a finding which was consistent with the findings of this study.
This test revealed that the studied participants with aphasia performed more poorly in selective attention than the subjects of the control group. The attention subtest was significantly correlated with 5 language subtests (phonological fluency, reading, auditory comprehension, & writing to dictation) in the aphasia group. There were no significant differences between the patients and controls regarding the subtests of memory and reasoning. In the PWA group, each of these two subtests was significantly correlated with only one subtest of the language section. However, cognitive functions were correlated mainly with the color-shape test, phonological and semantic fluency, naming, reading aloud, reading comprehension, and auditory comprehension in the control group. These findings were in a completely reverse correlation with those of the original study on the test; there was a low correlation between the subtests of cognition and language in the control group. However, there was a high correlation between these two sections in the aphasia group. One reason could be the number of patients, which was too small to show a higher correlation in the group. Therefore, more studies should be conducted on larger samples, including more diverse aphasia types.
5. Conclusion
The ACL-P test is reliable and valid for use in early evaluations, detecting progress throughout treatment courses, and prioritizing therapeutic goals in clinical environments. It can also be employed in experimental studies on aphasia in Persian.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the Tehran University of Medical Sciences (Code: IR.TUMS.VCR.REC.1395.1216).
Funding
The study was supported by the Tehran University of Medical Sciences.
Authors' contributions
Conceptualization, review and editing: Ahmad Reza Khatoonabadi; Writing original draft, performing the study: Amin Modarreszadeh; Review and editing: Azar Mehri; Data analysis, review: Shohreh Jalaei; Conceptualization, review and editing: Elke Kalbe.
Conflict of interest
The authors declared no conflicts of interest.
References
Benjamin, E. J., Blaha, M. J., Chiuve, S. E., Cushman, M., Das, S. R., & Deo, R., et al. (2017). Heart disease and stroke statistics-2017 update: A report from the American Heart Association. Circulation, 135(10), e146-603. [DOI:10.1161/CIR.0000000000000485] [PMID] [PMCID]
Berthier, M. L. (2005). Poststroke aphasia. Drugs & Aging, 22(2), 163-82. [DOI:10.2165/00002512-200522020-00006] [PMID]
Bruce, C., & Edmundson, A. (2010). Letting the CAT out of the bag: A review of the comprehensive aphasia test. Commentary on Howard, Swinburn, and Porter,”putting the CAT out: What the comprehensive aphasia test has to offer”. Aphasiology, 24(1), 79-93. [DOI:10.1080/02687030802453335]
Damico, J. S., Müller, N., & Ball, M. J., Eds. (2010). The handbook of language and speech disorders. Chichester: Blackwell Publishing. [DOI:10.1002/9781444318975]
Davidson, B., Howe, T., Worrall, L., Hickson, L., & Togher, L. (2008). Social participation for older people with aphasia: The impact of communication disability on friendships. Topics in Stroke Rehabilitation, 15(4), 325-40. [DOI:10.1310/tsr1504-325] [PMID]
Delazer, M., & Bartha, L. (2001). Transcoding and calculation in aphasia. Aphasiology, 15(7), 649-79. [DOI:10.1080/02687040143000104]
El Hachioui, H., Visch-Brink, E. G., Lingsma, H. F., van de Sandt-Koenderman, M. W. M. E., Dippel, D. W. J., & Koudstaal, P. J., et al. (2014). Nonlinguistic cognitive impairment in poststroke aphasia: A prospective study. Neurorehabilitation and Neural Repair, 28(3), 273-81. [DOI:10.1177/1545968313508467] [PMID]
Engelter, S. T., Gostynski, M., Papa, S., Frei, M., Born, C., & Ajdacic-Gross, V., et al. (2006). Epidemiology of aphasia attributable to first ischemic stroke: Incidence, severity, fluency, etiology, and thrombolysis. Stroke, 37(6), 1379-84. [DOI:10.1161/01.STR.0000221815.64093.8c] [PMID]
Godecke, E., Ciccone, N. A., Granger, A. S., Rai, T., West, D., & Cream, A., et al. (2014). A comparison of aphasia therapy outcomes before and after a Very Early Rehabilitation programme following stroke. International Journal of Language & Communication Disorders, 49(2), 149-61. [DOI:10.1111/1460-6984.12074] [PMID]
Hallowell, B., & Chapey, R. (2008). Introduction to language intervention strategies in adult aphasia. Philadelphia, PA: Lippincott, Williams, & Wilkins. https://www.researchgate.net/publication/277955261_Introduction_to_language_intervention_strategies_in_adult_aphasia
Kalbe, E., Reinhold, N., Brand, M., Markowitsch, H. J., & Kessler, J. (2005). A new test battery to assess aphasic disturbances and associated cognitive dysfunctions - German normative data on the aphasia check list. Journal of Clinical and Experimental Neuropsychology, 27(7), 779-94. [DOI:10.1080/13803390490918273] [PMID]
Kauhanen, M. L., Korpelainen, J. T., Hiltunen, P., Määttä, R., Mononen, H., & Brusin, E., et al. (2000). Aphasia, depression, and non-verbal cognitive impairment in ischaemic stroke. Cerebrovascular Diseases, 10(6), 455-61. [DOI:10.1159/000016107] [PMID]
Laska, A. C., Hellblom, A., Murray, V., Kahan, T., & Von Arbin, M. (2001). Aphasia in acute stroke and relation to outcome. Journal of Internal Medicine, 249(5), 413-22. [DOI:10.1046/j.1365-2796.2001.00812.x] [PMID]
Lum, C., & Ellis, A. W. (1999). Why do some aphasics show an advantage on some tests of nonpropositional (automatic) speech? Brain and Language, 70(1), 95-118. [DOI:10.1006/brln.1999.2147] [PMID]
Luzzatti, C., Toraldo, A., Zonca, G., Cattani, B., & Saletta, P. (2006). Types of dyslexia in aphasia: A multiple single-case study in a shallow orthography language. Brain and Language, 99(1-2), 28-9. [DOI:10.1016/j.bandl.2006.06.024]
Mayer, J. F., & Murray, L. L. (2012). Measuring working memory deficits in aphasia. Journal of Communication Disorders, 45(5), 325-39. [DOI:10.1016/j.jcomdis.2012.06.002] [PMID]
Murray, L. L. (2012). Attention and other cognitive deficits in aphasia: Presence and relation to language and communication measures. American Journal of Speech-Language Pathology, 21(2). [DOI:10.1044/1058-0360(2012/11-0067)]
Murray, L. L. (2017). Design fluency subsequent to onset of aphasia: A distinct pattern of executive function difficulties? Aphasiology, 31(7), 793-818. [DOI:10.1080/02687038.2016.1261248]
Patterson, J. P., & Chapey, R. (2008). Assessment of language disorders in adults. In: R. Chapey., Language intervention strategies in aphasia and related neurogenic communication disorders (5th ed., pp. 64-152). Philadelphia, PA: Lippincott Williams & Wilkins.
Nilipour, R., Pourshahbaz, A., & Ghoreyshi, Z. S. (2014). Reliability and validity of bedside version of Persian WAB (P-WAB-1). Basic and Clinical Neuroscience, 5(4), 253-8. [PMID] [PMCID]
Rossor, M. N., Warrington, E. K., & Cipolotti, L. (1995). The isolation of calculation skills. Journal of Neurology, 242(2), 78-81. [DOI:10.1007/BF00887820] [PMID]
Sachdev, P. S., Blacker, D., Blazer, D. G., Ganguli, M., Jeste, D. V., & Paulsen, J. S., et al. (2014). Classifying neurocognitive disorders: The DSM-5 approach. Nature Reviews Neurology, 10(11), 634-42. [DOI:10.1038/nrneurol.2014.181] [PMID]
Seyedian, M., Falah, M., Nourouzian, M., Nejat, S., Delavar, A., & Ghasemzadeh, H. A. (2008). [Validity of the Farsi version of mini-mental state examination (Persian)]. Journal of Medical Council of Iran, 25(4), 408-14. http://jmciri.ir/article-1-1170-fa.html
Soltani, Sh., Khatoonabadi, A. R., Jenabi, M. S., & Piran, A. (2013). Frequency of aphasia resulting from stroke at hospitals affiliated to Tehran University of Medical Sciences. Journal of Modern Rehabilitation, 6(4), 44-8. https://www.magiran.com/paper/1101712
Spreen, O., & Risser, A. H. (2003). Purposes of assessment. In O. Spreen & A. H. Risser. Assessment of aphasia (pp. 22-29). New York: Oxford University Press. https://books.google.com/books?id=fBRnDAAAQBAJ&dq
Vallila-Rohter, S., & Kiran, S. (2013). Non-linguistic learning and aphasia: Evidence from a paired associate and feedback-based task. Neuropsychologia, 51(1), 79-90. [DOI:10.1016/j.neuropsychologia.2012.10.024] [PMID] [PMCID]
Villard, S., & Kiran, S. (2015). Between-session intra-individual variability in sustained, selective, and integrational non-linguistic attention in aphasia. Neuropsychologia, 66, 204-12. [DOI:10.1016/j.neuropsychologia.2014.11.026] [PMID]
Ware Jr, J. E., & Gandek, B. (1998). Overview of the SF-36 health survey and the International Quality of Life Assessment (IQOLA) project. Journal of Clinical Epidemiology, 51(11), 903-12. [DOI:10.1016/S0895-4356(98)00081-X]
Zamani, P., & Madjdinasab, N. (2013). [Time variation in the occurrence of stroke-induced aphasia: A report from Ahvaz (Persian)]. Medical Journal of Tabriz University of Medical Sciences, 35(2), 44-9. https://mj.tbzmed.ac.ir/Article/8507
Aphasia is an acquired disorder of verbal communication. It always occurs due to some damage to certain parts of the brain responsible for speech and language processing. It is mainly manifested by impairments in the receptive and expressive modalities of spoken and written language to different extents (Hallowell & Chapey, 2008). Moreover, the deficits of memory (Vallila-Rohter & Kiran, 2013; Mayer & Murray, 2012), attention (Murray, 2012; Villard & Kiran), reasoning (Murray, 2012), and executive functions (Murray, 2017) can be comorbid with aphasia. Cerebrovascular accident is the most prevalent cause of aphasia. Ischemic infarction causes 80% of aphasic cases (Berthier, 2005). According to the studies conducted in Europe and the US, one-third of all patients with stroke are prone to aphasia in acute stages (Damico, Müller & Ball, 2010; Engelter et al., 2006; Laska, Hellborn, Murray, Kahan, & Von Arbin, 2001). In Iran, two studies examined the prevalence of aphasia. A cross-sectional study indicated that 5 out of 22 stroke patients (equal to 22.7% of the statistical population) had aphasia (Soltani, Khatoonabadi, Jenabi, & Piran, 2013). A retrospective study revealed that 727 out of 1817 such patients (equal to 39.9% of the statistical population) had a particular type of aphasia (Zamani & Madjdinasab, 2013). The relatively high prevalence of aphasia among patients with a first-ever stroke adversely affects the affected individuals’ quality of life respecting depression and social isolation (Kauhanen et al., 2000; Davidson, Howe, Worrall, Hickson, & Togher, 2008). Thus, it seems necessary to implement early intervention programs (Godecke et al., 2014); the first step of which is evaluation (Papathanasiou, Coppens, & Potagas, 2012). Evaluation can be conducted for various purposes as determining the presence of aphasia and its classification; the severity of the disorder; the nature of the observed language disorders; setting therapeutic objectives and adopting adequate approaches; treatment prognosis, and changes in the treatment process (Bruce & Edmundson, 2010). One aphasia test alone cannot meet all of the above-mentioned goals. Therefore, clinicians were advised to reflect on the exact purpose of their examination before choosing assessment tools (Spreen & Risser, 2003). When a therapist intends to collect samples from various verbal behaviors at different levels of assignment difficulty in the expressive and receptive modalities, comprehensive aphasia tests should be used (Patterson & Chapey, 2008).
The Persian Aphasia Test is the only comprehensive scale released in Iran. It evaluates the 6 primary language skills, i.e., oral expression, oral comprehension, repetition, available vocabulary, reading, and writing. According to the developers, this test was used by speech and language pathologists for over 20 years within the country; however, its use may cause problems. This test consists of 25 subtests and 217 items. Thus, it might be time-consuming and tiring when conducted on an aphasic population because aphasia occurs mostly after the age of 65 years (Benjamin et al., 2017). Accordingly, patients may not be cooperative. As discussed earlier, aphasia is a multifaceted disorder that can affect other language-dependent aspects of cognitive functioning, such as non-word processing (Luzzatti, Toraldo, Zonca, Cattani, & Saletta, 2006), numerical processing (Delazer & Bartha, 2001), and neuropsychological abilities including memory, attention, and reasoning (Murray, 2012; El Hachioui et al., 2014). Therefore, a comprehensive aphasia test should also cover these areas. Accordingly, the authors of this paper decided to translate the ACL, i.e., a German aphasia test, and evaluate its psychometric features. The ACL has certain advantages, the most important of which is that it takes 30-40 minutes to administer the entire test. This feature enables the therapist to finish the evaluation process in one session; therefore, respondents will experience less fatigue. Another feature of this test is that it uses various verbal stimuli [sentences, words (nouns & verbs), non-words, & numbers] for language evaluation. These stimuli become systematically complicated every task, something which can significantly help in pinpointing the examinee’s level of performance. Moreover, to minimize the interference of a faulty language system during the cognitive assessment, nonverbal stimuli were used in the cognition part of the test (Kalbe, Reinhold, Brand, Markowitsch, & Kessler, 2005). This test was provided with cut-off points per subtest in the language and cognition sections to evaluate the presence of disorder in the respective area of functioning; also a total cut-off point is determined for determining the presence of aphasia in the language section. It is easy to conduct and has a convenient scoring method. Therefore, it appeared that translating and publishing this test could greatly help Iranian therapists to increase the quality of intervention offered to PWA.
2. Methods
Initially, permission to translate the test to Persian was obtained from the test developer. Then, the translation process began based on the International Quality of Life Assessment (IQOLA) protocol for standard translation (Ware & Gandek, 1998).
Phase 1: The German-to-Persian translation process was started by two Persian-speaking translators (Translator 1 and Translator 2). These two translators mastered languages and linguistics terms and concepts. However, they were unfamiliar with the ACL test, and each one independently translated the test.
Phase 2: After finishing the forward translation process, each translator was requested to score all sections translated by the other translator (words, expressions, & sentences) concerning difficulty using a 100-point Likert-type scale, in which 0 indicate completely understandable, and 100 reflect unintelligibly. If an item was scored above 30, it would be considered hard, then returned to its translator. In this section, none of the items was scored above 30.
Phase 3: In this phase, two other bilingual translators were requested to score the quality of each version of the translations. By quality, we mean the simplicity and clarity of translation. These translators had no connection to translators 1 and 2 and lacked clinical experience. They independently gave scores from each other. Again, a 100-point visual scale was employed. On this scale, 0 addressed the lowest quality of translation, and 100 indicated the highest. With a score <90, the translation was considered low-quality with the need for revision by its translator. In this phase, none of the items received a score below 90.
Phase 4: In this phase, an expert panel was held for translators 1 and 2, and the researchers to evaluate and compare the difficulty and quality of the translations. At last, one translation was agreed upon.
Phase 5: The final translated version of the ACL in Persian was back-translated by another translator (translator 5) into German. This translator had not been present in the previous phases and knew nothing about the purpose and intended use of the ACL.
Phase 6: After finishing the back-translation, the original version of the test was compared with the back-translated version by an expert panel for any necessary corrections or revisions. Finally, a satisfactory Persian version of the text was reached.
Phase 7: Ten speech and language pathologists working in the field of aphasia management were requested to score the pre-final Persian version concerning its following the required criteria using a 4-point Likert-type scale respecting the comprehensibility of the commands and stimuli; the sociocultural suitability of the test stimuli; and the clarity and fluency of the used words, expressions, and sentences. On this scale, 0 reflected the absence of the criteria as mentioned earlier, and 4 reflected full compliance with them. If 80% of the respondents gave <3 to any item, it had to be sent to the corresponding translator for revision. All of the verbal items received acceptable scores. The expert panel confirmed the adequacy of the results of this field testing, and the Persian version of the ACL (called ACL-P from now on) was prepared to be evaluated among a population of PWA.
In this study, the required PWAs were recruited based on the following criteria from the caseload of clinics affiliated with Tehran University of Medical Sciences through the convenience sampling method. The inclusion criteria were a first left-hemisphere stroke caused aphasia, and there had been no other previous strokes; at least 3months had passed since the stroke before the initiation of the study; the maximum age of 65 years; the native language had to be Persian, and the participant had to be literate before the occurrence of the lesion; no comorbid neurodegenerative or psychiatric diseases (e.g., dementia of Alzheimer’s type or clinical depression) based on their medical history, their prescribed medications and caregivers’ reports of their problems; participants had not received speech/language interventions at least one week before the testing sessions (they had already completed a program or were awaiting to be enrolled in a new program, or for whatever reason did not intend to take part in the speech therapy facilities available to them.
However, if they were receiving any program, they were excluded from this study. In addition to the usual evaluations of speech therapy, an experienced neurologist was available to confirm the diagnosis of aphasia. Neurologically, healthy controls were selected from the clients referred to the same clinics. They were the caretakers of participant patients or had other complaints than speech and language disorders (e.g., optometric & lower-back problems). The inclusion criteria for healthy participants were no history of verbal or cognitive disorders (diagnosed through the Persian version of MMSE; cut-off point= 23) (Seyedian et al., 2008); the lack of any biopsychological disorders disrupting test implementation; Persian as their native language (or using Persian as their preferred language in case of being bi/multilingual); being adequately literate to meet daily needs.
The research goals were explained to all study participant and their caretakers. Then, they were requested to sign an informed written consent, i.e., securely stored by one of the researchers.
The ACL-P was individually provided to the research participant. The test was conducted in an acoustic well-lit room at the Rehabilitation School of Tehran University of Medical Sciences, away from any visual distractions. If a participant could not attend this location for any reason, the testing sessions were pursued at their home per standard conditions. The language learning section was implemented by asking oral questions or showing pictures/printed words and recording responses. The cognitive section was paper-based. The study participants had to cross out the target items in the attention subtest. Moreover, PWAs used their non-dominant left hands to complete the task. Thus, before implementing the test in this group, they practiced crossing out geometrical items, such as squares and triangles with pencils to concentrate on the test instead of figuring out how to complete the task. The oral responses were immediately transcribed. However, these responses were also recorded by a device (Sony SO-ICD-PX240 4GB Voice Recorder). The retest session was held 10 days after the first testing session per study participant by the same examiner in the same conditions.
The ACL-P consists of two general sections; language and cognition. The language section consists of the following 7 subtests, used to evaluate the primary modalities of verbal comprehension and expression, reading, writing, and repetition, as follows: serial speech (2 tasks); following commands (2 tasks); the color-shape test; word generation (2 tasks); specific verbal abilities: a) confrontation naming; b) reading aloud; c) reading comprehension; d) listening comprehension; e) writing to dictation; f) repetition (45 tasks); evaluation of general verbal communication ability, and numerical processing (3 tasks). The cognitive section consists of 3 subtests i.e., memory, attention, and reasoning. Regarding the memory subtest, the participants looked at 6 geometrical shapes for 10 seconds. Then, they were requested to recognize them among an assortment of shapes immediately (short-term memory) and after 10 minutes (mid-term memory). The attention section was designed to evaluate the speed and quality of selective attention through a task of canceling out two geometrical shapes in a block of similar shapes. Regarding reasoning, there were 11 sequences of 9 objects, 8 of which were arranged according to a rule, and the examiner must determine the one that disrupted the arrangement (Kalbe et al., 2005).
The resultant data were analyzed in SPSS. The Shapiro-Wilk test was conducted to check the normality of data. The Mann-Whitney U test was performed to evaluate the discriminant validity. The ICC coefficients (an absolute agreement, two-way mixed) were employed to determine the test-retest reliability of the scale. The lowest acceptable coefficient was considered 0.5, and values ranging between 0.5 and 0.75, between 0.75 and 0.9, and over 0.9 were respectively considered mediocre, good, and excellent. Cronbach’s alpha coefficient was employed to analyze the internal consistency of the scale. The coefficients ranging between 0.7 and 0.9 were regarded as excellent. The Spearman rank correlation coefficient test was implemented to determine the correlation between the language and cognition parts of the test. The minimum and maximum scores were considered to determine the floor and ceiling effects, respectively. The floor and ceiling effects were significant if they were observed to be over 15%.
3. Results
In this study, the statistical population included 20 PWA (13 males & 7 females with the Mean±SD age of 56.90±7.51 years & the age range of 45-65 years) and 50 neurologically healthy individuals (29 males & 21 females with the Mean±SD age of 59.80±5.20 years and the age range of 52-70 years). The Mean±SD years of education in the patient and control groups were 11.85±3.94 years (range: 5-18 years) and 11.34±3.79 years (range: 4-18 years). According to the Shapiro-Wilk test results, age followed no normal distribution in the patient group (W= 0.864 & P= 0.009) and the control group (W= 0.939 & P= 0.013). The educational attainment had a normal distribution in the patient group (W= 0.905 & P= 0.052); however, it suggested a significant difference from the normal distribution in the control group (W= 0.906 & P= 0.001). There was no significant difference between the study groups concerning age (U= 408 & P= 0.230) and education (U= 455 & P= 0.543). The Mean±SD score of the elapsed time from the onset of the disorder to the initiation of the study was measured as 29.7±17.89 months, with a range of 8-60 months in the patient group. Based on hospital discharge records, MRI scans, and language evaluations via the P-WAB-1 test (Nilipour, Pourshahbaz, & Ghoryshi, 2014), the type of aphasia was categorized in all the subjects as non-fluent. It was due to lesions to the perisylvian areas of the left hemisphere. In the control group, the MMSE test was conducted to evaluate mental health. Their Mean±SD scores were 27.76±2.20, with a range of 24-30.
The total scores of all language assignments of the ACL-P were 213. For the language section of the test, the means and ranges of the total scores in the test (Mean±SD= 112.7±7.58 & range= 63-171) and retest (Mean±SD= 120.35±7.20 & range= 69-174) sessions reflected no floor and ceiling effects. The distribution of scores was normal in the patient group in the test (W= 0.935 & P= 0.191) and the retest (W= 0.952 & P= 395) phases. According to the test’s manual, 8 subtests (phonological fluency, semantic fluency, listening comprehension, reading comprehension, naming, reading aloud, the dictation of words & sentences, the repetition of words & sentences, & color-shape test) were considered the essential subtests (these subtests are henceforth called diagnostic subtests). The maximum total score for these subtests was 148. The scores of the patient group presented no such effects in the test (Mean±SD= 78.10±24.01; range=44-115) and the retest (Mean±SD= 82.5±22.75; range=42-120) for the diagnostic subtests. The distribution of scores was normal in the test (W= 907 & P= 0.56) and the retest (W= 0.952 & P= 0.395). Given that the constructs are dependent on each other in the cognition part of the ACL-P, the scores of this section cannot be added together.
Therefore, each subtest’s score was reported separately for this part of the test. No floor and ceiling effects were observed for immediate memory (mean=4.45; range= -1 to 6) in the test and in the retest sessions (mean= 4.95; range= 3-6); also the case for delayed memory in the test (mean= 3.95; range= 2-6) and the retest (mean= 4.3; range= 2-6) sessions (the minimum score was -6 on this subtest). In the attention section, 3 scores were determined: the total number of processed items (144 at most), the differentiation of the processed items and errors (no maximum), and error frequency (66.6% at most). There were no floor and ceiling effects either for the total number of processed items in the test (mean= 61; range= 25-117) or the retest (mean= 56.5; range=24-110) nor were there any for the error percentage in the test (mean= 5.14; range= 0-22.2) and the retest (mean= 5.07; range= 0-15.6) sessions. Regarding the subtest of reasoning (the maximum score equaled 11), the same was true in the test (mean= 5.8, range= 4-10) and the retest (mean= 6; range= 4-10) sessions. The next section addresses the floor and ceiling effects on each subtest.
There were significant differences between the total score of the language section (Mann–Whitney U= 6.000, n1= 50, n2= 20, P<0.001) and the scores of diagnostic subtests (Mann–Whitney U=3.000, n1= 50, n2= 20, P<0.001) for the control and PWA groups. Table 1 presents the control and patient scores on each subtest of the ACL-P in the first execution of the test.
.png)
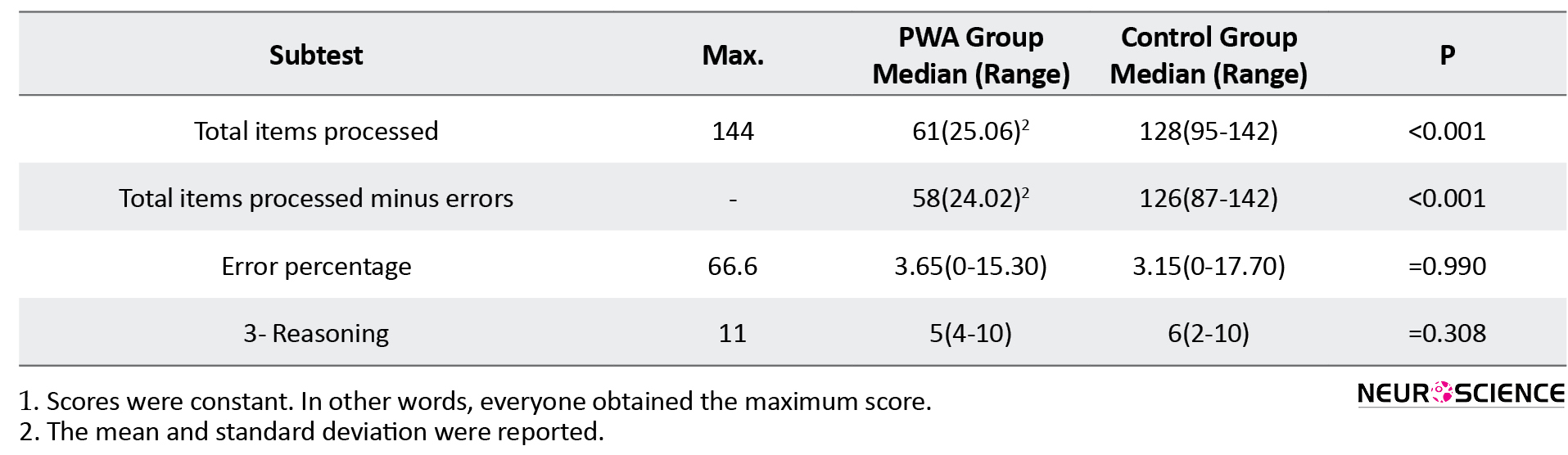
It also outlines the significance of the difference between the mean or median scores of these two groups. The results of most of these subtests did not follow a normal distribution in the patient and control groups; thus, the medians and score ranges were reported. If the scores follow a normal distribution, the mean and standard deviation are reported and highlighted. Accordingly, the research groups were significantly different from each other on all subtests of the language section. In the second section of the test, a significant difference was only observed in the subtest of attention. Cronbach’s alpha coefficient method was employed to test the internal consistency. The obtained coefficient was 0.761 for the entire test (both language and cognition sections were considered) in both test and retest phases. The values of Cronbach’s alpha coefficient ranged from 0.777 to 0.804 in the test phase and from 0.727 to 0.895 in the retest phase in case of item deletion. Cronbach’s alpha coefficient was calculated as 0.884 (ranged, if item deleted, from 0.867 to 0.884) for the language part and was measured to be 0.071 (ranged, if item deleted, from 0.060 to 0.563) for the cognition part in the test phase. These values were 0.899 (range= 0.878-904) for the language part and 0.120 (range= 0.052-0.123) for the cognition part in the retest. Regarding the diagnostic subtests of the language section, Cronbach’s alpha coefficient was computed as 0.852 in the test phase. However, it equaled 0.878 in the retest phase. If items were deleted, the coefficient ranged from 0.809 to 0.859 in the test phase and from 0.838 to 0.898 in the retest phase.
The value of ICCagreement was high for the total scores of the language section (ICC agreement= 0.982, 95%CI= 0.819-0.995, P<0.001). It was also high in the diagnostic subtests (ICCagreement= 0.981, 95%CI= 0.863-0.995, P<0.001). Table 2 manifests the values of ICCagreement determined for every ACL subtest in the language and cognition sections.
.png)
Accordingly, ICC was acceptable with a 95% confidence interval in all ACL-P subtests. More precisely, it ranged between 0.573 and 0.984 at a significance level of P<0.05.
As discussed earlier, the ACL-P test consists of two sections; language and cognition. According to the cognition part data, all of the surveyed patients had dysfunctions in at least one of the cognitive areas [short memory, midterm memory, attention (the total processed items minus errors), and reasoning]. A Performance lower than the cut-off points was observed in 4 participants on one subtest, in 9 participants on two subtests, in 3 participants on three subtests, and 4 participants on four subtests. The frequency of the presence of disorder in each domain was as follows: attention (19 participants), reasoning (15 participants), short-term memory (7 participants), and midterm memory (6 participants). Moreover, Table 3 indicates the values of correlation between the essential subtests of the language section and the subtests of the cognition section in the healthy and aphasic groups.
.png)
Accordingly, the number of significant correlations in the control group was more extensive than that of the PWA group. In the control group, the only subtest without correlations with the cognition subtests was repetition. In the patient group, the color-shape and repetition subtests had no correlations with any of the cognition subtests. The subtest of attention had the most significant number of correlations with the language subtests.
4. Discussion
This study aimed at the cultural adaptation and determination of the psychometric features of the ACL-P test. Accordingly, it could be used for evaluation purposes in Persian-speaking clinical environments where persons with aphasia attend. The coverage of a wide variety of language skills and the relatively short administration time make this test suitable for a time-saving but comprehensive assessment. The subtests include different numbers of tasks proportional to their relevance to the main characteristics of aphasia. For instance, the subtest for comprehension of words/sentences (i.e., essential for diagnosis and classification of aphasia syndromes) consisted of 6 tasks. In contrast, the subtest for reading numbers included three assignments. As a result, the therapist can screen lesser-important language skills and conduct a more comprehensive evaluation of these skills, only if it becomes necessary. The presence of nonverbal assignments for assessing short-term memory, midterm memory, attention, and reasoning are among the other hallmarks of this test. According to recent studies, cognitive functions can affect the evaluation process and the response to treatment. Therefore, it is essential to understand a patient’s cognitive status (Villard & Kiran, 2015).
The translation process was performed smoothly because a standard protocol was employed for translation. Furthermore, the stimuli and guidelines in the source language (German) were void of any linguistic complexity (e.g., the usage of words with multiple meanings or long sentences); the face and content validities of the test was appropriate. However, a few changes were made in the verbal stimuli of the test and pictures. As for the reading, repeating, and writing of non-words, the test items matching the Persian phonotactic constraints were used. The pictures used for naming and reading comprehension were changed to match the Islamic culture governing Iran (Figure 1).
.png)
Moreover, all of the other items matched the Persian language and Iranian culture.
As a group, the study participants with aphasia did not obtain the minimum and maximum scores in any subtest of ACL-P during the test and retest sessions. The analysis of every subtest of the language section found that several participants in the aphasia group did obtain maximum scores in the subtests of automatic speech, following commands, and numerical processing in the test and retest phases. One reason could be the type of aphasia. Auditory comprehension is usually damaged less than other language functions in nonfluent aphasia. This was the type presented by all aphasic patients in the current study; therefore, the maximum score was observed in the direction-following subtest. The satisfactory performance of some aphasic participants in the automatic speech subtest (including reciting the days of the week & counting to 15) was consistent with the fact that PWA presents better performances in non-propositional (automatic) language than in propositional language assignments (Lum & Ellis, 1999). Regarding the maximum score of the numerical processing subtests, the collected results were consistent with the evidence that there can be distinctions between verbal functions and numerical processing functions of aphasic patients (Rossor, Warrington, & Cipolotti, 1995). In the original paper introducing this test, the score range of reading, writing, and repeating numbers were between 0 and 9, indicating that some patients with the disorder may reach the maximum score in these subtests (Kalbe et al., 2005).
According to the Cronbach alpha coefficients of all subtests and diagnostic subtests, the ACL-P had an acceptable internal consistency. In the original paper of the test, the values of Cronbach’s alpha coefficient were reported to range between 0.4 and 0.88 (Kalbe et al., 2005). Lower internal consistency of the cognition part of the ACL-P, compared to that of the language part, was expected. This is because it consisted of distinct cognitive domains of memory, attention, and reasoning (Sachdev et al., 2014). Moreover, this test demonstrated acceptable test-retest reliability. In the original normative study of the ACL, the test-retest reliability ranged between 0.5 and 0.91 at P<0.05; a finding which was consistent with the findings of this study.
This test revealed that the studied participants with aphasia performed more poorly in selective attention than the subjects of the control group. The attention subtest was significantly correlated with 5 language subtests (phonological fluency, reading, auditory comprehension, & writing to dictation) in the aphasia group. There were no significant differences between the patients and controls regarding the subtests of memory and reasoning. In the PWA group, each of these two subtests was significantly correlated with only one subtest of the language section. However, cognitive functions were correlated mainly with the color-shape test, phonological and semantic fluency, naming, reading aloud, reading comprehension, and auditory comprehension in the control group. These findings were in a completely reverse correlation with those of the original study on the test; there was a low correlation between the subtests of cognition and language in the control group. However, there was a high correlation between these two sections in the aphasia group. One reason could be the number of patients, which was too small to show a higher correlation in the group. Therefore, more studies should be conducted on larger samples, including more diverse aphasia types.
5. Conclusion
The ACL-P test is reliable and valid for use in early evaluations, detecting progress throughout treatment courses, and prioritizing therapeutic goals in clinical environments. It can also be employed in experimental studies on aphasia in Persian.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the Tehran University of Medical Sciences (Code: IR.TUMS.VCR.REC.1395.1216).
Funding
The study was supported by the Tehran University of Medical Sciences.
Authors' contributions
Conceptualization, review and editing: Ahmad Reza Khatoonabadi; Writing original draft, performing the study: Amin Modarreszadeh; Review and editing: Azar Mehri; Data analysis, review: Shohreh Jalaei; Conceptualization, review and editing: Elke Kalbe.
Conflict of interest
The authors declared no conflicts of interest.
References
Benjamin, E. J., Blaha, M. J., Chiuve, S. E., Cushman, M., Das, S. R., & Deo, R., et al. (2017). Heart disease and stroke statistics-2017 update: A report from the American Heart Association. Circulation, 135(10), e146-603. [DOI:10.1161/CIR.0000000000000485] [PMID] [PMCID]
Berthier, M. L. (2005). Poststroke aphasia. Drugs & Aging, 22(2), 163-82. [DOI:10.2165/00002512-200522020-00006] [PMID]
Bruce, C., & Edmundson, A. (2010). Letting the CAT out of the bag: A review of the comprehensive aphasia test. Commentary on Howard, Swinburn, and Porter,”putting the CAT out: What the comprehensive aphasia test has to offer”. Aphasiology, 24(1), 79-93. [DOI:10.1080/02687030802453335]
Damico, J. S., Müller, N., & Ball, M. J., Eds. (2010). The handbook of language and speech disorders. Chichester: Blackwell Publishing. [DOI:10.1002/9781444318975]
Davidson, B., Howe, T., Worrall, L., Hickson, L., & Togher, L. (2008). Social participation for older people with aphasia: The impact of communication disability on friendships. Topics in Stroke Rehabilitation, 15(4), 325-40. [DOI:10.1310/tsr1504-325] [PMID]
Delazer, M., & Bartha, L. (2001). Transcoding and calculation in aphasia. Aphasiology, 15(7), 649-79. [DOI:10.1080/02687040143000104]
El Hachioui, H., Visch-Brink, E. G., Lingsma, H. F., van de Sandt-Koenderman, M. W. M. E., Dippel, D. W. J., & Koudstaal, P. J., et al. (2014). Nonlinguistic cognitive impairment in poststroke aphasia: A prospective study. Neurorehabilitation and Neural Repair, 28(3), 273-81. [DOI:10.1177/1545968313508467] [PMID]
Engelter, S. T., Gostynski, M., Papa, S., Frei, M., Born, C., & Ajdacic-Gross, V., et al. (2006). Epidemiology of aphasia attributable to first ischemic stroke: Incidence, severity, fluency, etiology, and thrombolysis. Stroke, 37(6), 1379-84. [DOI:10.1161/01.STR.0000221815.64093.8c] [PMID]
Godecke, E., Ciccone, N. A., Granger, A. S., Rai, T., West, D., & Cream, A., et al. (2014). A comparison of aphasia therapy outcomes before and after a Very Early Rehabilitation programme following stroke. International Journal of Language & Communication Disorders, 49(2), 149-61. [DOI:10.1111/1460-6984.12074] [PMID]
Hallowell, B., & Chapey, R. (2008). Introduction to language intervention strategies in adult aphasia. Philadelphia, PA: Lippincott, Williams, & Wilkins. https://www.researchgate.net/publication/277955261_Introduction_to_language_intervention_strategies_in_adult_aphasia
Kalbe, E., Reinhold, N., Brand, M., Markowitsch, H. J., & Kessler, J. (2005). A new test battery to assess aphasic disturbances and associated cognitive dysfunctions - German normative data on the aphasia check list. Journal of Clinical and Experimental Neuropsychology, 27(7), 779-94. [DOI:10.1080/13803390490918273] [PMID]
Kauhanen, M. L., Korpelainen, J. T., Hiltunen, P., Määttä, R., Mononen, H., & Brusin, E., et al. (2000). Aphasia, depression, and non-verbal cognitive impairment in ischaemic stroke. Cerebrovascular Diseases, 10(6), 455-61. [DOI:10.1159/000016107] [PMID]
Laska, A. C., Hellblom, A., Murray, V., Kahan, T., & Von Arbin, M. (2001). Aphasia in acute stroke and relation to outcome. Journal of Internal Medicine, 249(5), 413-22. [DOI:10.1046/j.1365-2796.2001.00812.x] [PMID]
Lum, C., & Ellis, A. W. (1999). Why do some aphasics show an advantage on some tests of nonpropositional (automatic) speech? Brain and Language, 70(1), 95-118. [DOI:10.1006/brln.1999.2147] [PMID]
Luzzatti, C., Toraldo, A., Zonca, G., Cattani, B., & Saletta, P. (2006). Types of dyslexia in aphasia: A multiple single-case study in a shallow orthography language. Brain and Language, 99(1-2), 28-9. [DOI:10.1016/j.bandl.2006.06.024]
Mayer, J. F., & Murray, L. L. (2012). Measuring working memory deficits in aphasia. Journal of Communication Disorders, 45(5), 325-39. [DOI:10.1016/j.jcomdis.2012.06.002] [PMID]
Murray, L. L. (2012). Attention and other cognitive deficits in aphasia: Presence and relation to language and communication measures. American Journal of Speech-Language Pathology, 21(2). [DOI:10.1044/1058-0360(2012/11-0067)]
Murray, L. L. (2017). Design fluency subsequent to onset of aphasia: A distinct pattern of executive function difficulties? Aphasiology, 31(7), 793-818. [DOI:10.1080/02687038.2016.1261248]
Patterson, J. P., & Chapey, R. (2008). Assessment of language disorders in adults. In: R. Chapey., Language intervention strategies in aphasia and related neurogenic communication disorders (5th ed., pp. 64-152). Philadelphia, PA: Lippincott Williams & Wilkins.
Nilipour, R., Pourshahbaz, A., & Ghoreyshi, Z. S. (2014). Reliability and validity of bedside version of Persian WAB (P-WAB-1). Basic and Clinical Neuroscience, 5(4), 253-8. [PMID] [PMCID]
Rossor, M. N., Warrington, E. K., & Cipolotti, L. (1995). The isolation of calculation skills. Journal of Neurology, 242(2), 78-81. [DOI:10.1007/BF00887820] [PMID]
Sachdev, P. S., Blacker, D., Blazer, D. G., Ganguli, M., Jeste, D. V., & Paulsen, J. S., et al. (2014). Classifying neurocognitive disorders: The DSM-5 approach. Nature Reviews Neurology, 10(11), 634-42. [DOI:10.1038/nrneurol.2014.181] [PMID]
Seyedian, M., Falah, M., Nourouzian, M., Nejat, S., Delavar, A., & Ghasemzadeh, H. A. (2008). [Validity of the Farsi version of mini-mental state examination (Persian)]. Journal of Medical Council of Iran, 25(4), 408-14. http://jmciri.ir/article-1-1170-fa.html
Soltani, Sh., Khatoonabadi, A. R., Jenabi, M. S., & Piran, A. (2013). Frequency of aphasia resulting from stroke at hospitals affiliated to Tehran University of Medical Sciences. Journal of Modern Rehabilitation, 6(4), 44-8. https://www.magiran.com/paper/1101712
Spreen, O., & Risser, A. H. (2003). Purposes of assessment. In O. Spreen & A. H. Risser. Assessment of aphasia (pp. 22-29). New York: Oxford University Press. https://books.google.com/books?id=fBRnDAAAQBAJ&dq
Vallila-Rohter, S., & Kiran, S. (2013). Non-linguistic learning and aphasia: Evidence from a paired associate and feedback-based task. Neuropsychologia, 51(1), 79-90. [DOI:10.1016/j.neuropsychologia.2012.10.024] [PMID] [PMCID]
Villard, S., & Kiran, S. (2015). Between-session intra-individual variability in sustained, selective, and integrational non-linguistic attention in aphasia. Neuropsychologia, 66, 204-12. [DOI:10.1016/j.neuropsychologia.2014.11.026] [PMID]
Ware Jr, J. E., & Gandek, B. (1998). Overview of the SF-36 health survey and the International Quality of Life Assessment (IQOLA) project. Journal of Clinical Epidemiology, 51(11), 903-12. [DOI:10.1016/S0895-4356(98)00081-X]
Zamani, P., & Madjdinasab, N. (2013). [Time variation in the occurrence of stroke-induced aphasia: A report from Ahvaz (Persian)]. Medical Journal of Tabriz University of Medical Sciences, 35(2), 44-9. https://mj.tbzmed.ac.ir/Article/8507
Type of Study: Original |
Subject:
Cognitive Neuroscience
Received: 2019/06/17 | Accepted: 2021/06/15 | Published: 2021/07/1
Received: 2019/06/17 | Accepted: 2021/06/15 | Published: 2021/07/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |